When Azoospermia Turns Your World Upside Down
Imagine eagerly planning for a family, dreaming of tiny hands and laughter, only to hear the words: “You have azoospermia.” Suddenly, your world feels like it’s spinning out of control. Azoospermia means no sperm is found in your semen, and for many, it’s not just a medical diagnosis—it’s a life-changing moment that shakes your dreams, relationships, and self-worth. You’re not alone, though. About 1% of all men and 10-15% of infertile men face this condition. But here’s the good news: there is hope, and we’re here to guide you through it.
In this article, we’ll explore everything you need to know about azoospermia, from what it is and how it’s diagnosed to the emotional toll it takes and the treatment options available. We’ll also dig into the latest research, share practical advice for coping, and offer ways to connect with support. Whether you’re a man facing this diagnosis, a partner trying to understand, or someone seeking answers, we’re here to provide clarity, support, and a path forward.
Introduction to Azoospermia
Azoospermia is a medical condition where a man’s semen contains no sperm. It’s a leading cause of male infertility, but it’s not always a dead end. Think of it like a roadblock on your journey to parenthood—there might be detours or new paths to explore. Let’s break it down.
What Is Azoospermia?
There are two main types of azoospermia:
-
- Obstructive azoospermia (OA): This happens when there’s a blockage in the reproductive tract, like a dam blocking a river. Sperm are being made, but they can’t get out. Common causes include:
-
- Being born without certain tubes (congenital abnormalities)
-
- Infections that scar the ducts
-
- Previous surgeries, like a vasectomy
-
- Obstructive azoospermia (OA): This happens when there’s a blockage in the reproductive tract, like a dam blocking a river. Sperm are being made, but they can’t get out. Common causes include:
-
- Non-obstructive azoospermia (NOA): This is when the testicles aren’t producing enough sperm. Imagine a factory that’s not making enough products. Causes can include:
-
- Genetic conditions, like Klinefelter syndrome
-
- Hormonal imbalances
-
- Damage from chemotherapy or injury
-
- Non-obstructive azoospermia (NOA): This is when the testicles aren’t producing enough sperm. Imagine a factory that’s not making enough products. Causes can include:
Understanding which type you have is key because it determines the treatments available. For OA, surgery might fix the blockage. For NOA, more advanced options, like sperm retrieval and IVF, could help.
How Common Is It?
Azoospermia affects:
-
- About 1% of all men
-
- 10-15% of men with infertility
It’s more common than you might think, and with today’s medical advancements, many men with azoospermia can still have biological children. But the journey isn’t just medical—it’s emotional, financial, and deeply personal.
Understanding the Diagnosis
Getting diagnosed with azoospermia can feel overwhelming, but understanding the process can help you feel more in control. Here’s what happens.
The Diagnostic Journey
-
- Semen Analysis:
-
- You’ll provide two semen samples, usually a few weeks apart.
-
- These are tested under a microscope. If no sperm are found after concentrating the sample (called centrifugation), azoospermia is confirmed.
-
- Why two tests? Sperm production can vary, and one test might not tell the whole story.
-
- Semen Analysis:
-
- Physical Exam:
-
- A doctor checks:
-
- Testicle size and feel (small or soft testicles might mean NOA)
-
- If the vas deferens (sperm-carrying tubes) are present
-
- Signs of hormonal issues, like enlarged breasts or lack of body hair
-
- A doctor checks:
-
- Physical Exam:
-
- Hormone Testing:
-
- Blood tests measure:
-
- Follicle-stimulating hormone (FSH): High levels might mean NOA.
-
- Luteinizing hormone (LH): Helps assess testicular function.
-
- Testosterone: Low levels could point to hormonal problems.
-
- Blood tests measure:
-
- Hormone Testing:
-
- Genetic Testing:
-
- Tests like karyotyping check for chromosomal abnormalities, like Klinefelter syndrome (47,XXY).
-
- Y-chromosome microdeletion analysis looks for missing genes that affect sperm production.
-
- Genetic Testing:
-
- Imaging:
-
- Ultrasounds can find:
-
- Blockages in the epididymis or ejaculatory ducts
-
- Varicoceles (enlarged veins that might impair sperm production)
-
- Missing structures, like seminal vesicles
-
- Ultrasounds can find:
-
- Imaging:
-
- Testicular Biopsy:
-
- If needed, a small piece of testicular tissue is removed and examined to see if sperm production is happening, even if it’s not reaching the semen.
-
- Testicular Biopsy:
Common Causes
Azoospermia can happen for many reasons, including:
-
- Genetic disorders: Like Klinefelter syndrome or Y-chromosome microdeletions.
-
- Hormonal imbalances: Problems with the brain’s signals to the testicles.
-
- Infections: Severe cases, like mumps orchitis, can damage the reproductive tract.
-
- Injury: Physical trauma to the testicles can impair function.
-
- Surgeries: Vasectomy, hernia repair, or prostate surgery can cause blockages.
-
- Toxins: Chemotherapy, radiation, or environmental pollutants can harm sperm production.
Emotional Reactions to Diagnosis
Hearing “azoospermia” can trigger a rollercoaster of emotions:
-
- Shock: “This can’t be happening to me.”
-
- Anger: “Why is this happening? It’s not fair.”
-
- Sadness: Grieving the loss of your fertility dreams.
-
- Anxiety: Worrying about costs, outcomes, and what others will think.
These feelings are normal and valid. It’s okay to grieve, and seeking support—from loved ones, therapists, or support groups—can make a big difference. Remember, you’re not alone.
Emotional Impact on Individuals and Couples
Azoospermia doesn’t just affect your body; it can shake your sense of self and strain relationships. Let’s explore how it impacts you and your partner, and how to cope.
Psychological Effects on Men
For many men, fertility is tied to masculinity and identity. Azoospermia can lead to:
-
- Feelings of inadequacy: “I’m not a real man if I can’t have kids.”
-
- Low self-esteem: Doubting your worth.
-
- Anxiety and depression: Constant worry or feelings of hopelessness.
-
- Guilt or shame: Blaming yourself for the couple’s infertility.
These emotions might show up as:
-
- Avoiding social events, especially baby showers or family gatherings
-
- Loss of interest in sex
-
- Trouble focusing at work or home
✔️ What to do:
-
- Talk to a therapist who understands infertility.
-
- Join a support group to connect with others who get it.
-
- Practice self-care, like exercising or journaling, to manage stress.
❌ What to avoid:
-
- Bottling up emotions—it can lead to more stress.
-
- Comparing yourself to others—it can deepen feelings of inadequacy.
Impact on Relationships and Intimacy
Azoospermia can strain even strong relationships. Couples might face:
-
- Communication breakdowns: Struggling to talk about feelings.
-
- Different coping styles: One partner wants to talk, the other needs space.
-
- Financial stress: Fertility treatments can be expensive.
-
- Intimacy issues: Sex might feel mechanical or tied to failure.
-
- Decision conflicts: Disagreeing on treatment options or family-building paths.
✔️ What to do:
-
- Set aside time to talk openly, using “I feel” statements (e.g., “I feel scared when we don’t talk about this”).
-
- Consider couples therapy to improve communication.
-
- Schedule date nights focused on connection, not conception.
-
- Join a support group for couples facing infertility.
❌ What to avoid:
-
- Blaming each other—it can erode trust.
-
- Ignoring intimacy—connection is key, even during tough times.
Coping Strategies
Here are some steps to help you and your partner navigate this journey:
-
- Acknowledge your feelings: It’s okay to feel sad, angry, or scared.
-
- Communicate openly: Share your fears and hopes with your partner.
-
- Seek professional help: A therapist can provide tools to cope.
-
- Connect with others: Support groups or online forums can reduce isolation.
-
- Practice self-care: Exercise, hobbies, and relaxation techniques can help.
Treatment Options
Azoospermia might feel like a dead end, but there are paths forward. Let’s explore treatments for both types, plus alternative family-building options.
Treatment for Obstructive Azoospermia (OA)
Since OA involves a blockage, treatments aim to remove or bypass it:
-
- Surgical repair:
-
- Procedures like vasovasostomy (reversing a vasectomy) or vasoepididymostomy (connecting tubes) can restore sperm flow.
-
- Success rates vary, but some men can conceive naturally after surgery.
-
- Surgical repair:
-
- Sperm retrieval:
-
- If surgery isn’t possible, sperm can be extracted from the testicles or epididymis using:
-
- Percutaneous epididymal sperm aspiration (PESA)
-
- Testicular sperm aspiration (TESA)
-
- If surgery isn’t possible, sperm can be extracted from the testicles or epididymis using:
-
- These sperm are then used in assisted reproductive technologies (ART).
-
- Sperm retrieval:
Treatment for Non-Obstructive Azoospermia (NOA)
NOA is trickier, but options exist:
-
- Hormone therapy:
-
- If hormonal imbalances are the cause, medications like gonadotropins can sometimes boost sperm production.
-
- Success depends on the underlying issue.
-
- Hormone therapy:
-
- Varicocele repair:
-
- Fixing enlarged veins in the scrotum might improve sperm production in some men.
-
- Varicocele repair:
-
- Surgical sperm retrieval:
-
- Techniques like testicular sperm extraction (TESE) or micro-TESE (using a microscope for precision) can find and extract sperm, even if production is low.
-
- Micro-TESE has a sperm retrieval rate of 45-50% for NOA, compared to 25-30% for regular TESE (Journal of Urology, 2023).
-
- Surgical sperm retrieval:
Assisted Reproductive Technologies (ART)
Once sperm are obtained, ART can help achieve pregnancy:
-
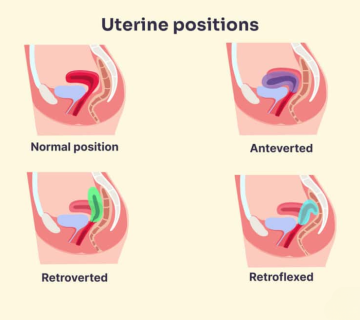
- In vitro fertilization (IVF):
-
- Eggs are fertilized in a lab, and embryos are implanted in the uterus.
-
- Often paired with ICSI for azoospermia cases.
-
- In vitro fertilization (IVF):
-
- Intracytoplasmic sperm injection (ICSI):
-
- A single sperm is injected into an egg, ideal when sperm count is low.
-
- Live birth rates for micro-TESE and ICSI are around 20-30% per cycle for NOA.
-
- Intracytoplasmic sperm injection (ICSI):
Alternative Family-Building Options
If biological parenthood isn’t possible or desired, consider:
-
- Donor sperm:
-
- Using sperm from a donor for artificial insemination or IVF.
-
- Discuss ethical, emotional, and legal aspects with your partner.
-
- Donor sperm:
-
- Adoption:
-
- Providing a loving home for a child in need.
-
- Research costs, timelines, and emotional considerations.
-
- Adoption:
-
- Child-free living:
-
- Embracing life without children, focusing on other goals and relationships.
-
- Explore ways to find fulfillment and joy.
-
- Child-free living:
✔️ Tips for choosing:
-
- Discuss all options openly with your partner.
-
- Consider counseling to explore your feelings.
-
- Research costs and insurance coverage for each path.
❌ What to avoid:
-
- Rushing into decisions—take time to weigh pros and cons.
-
- Ignoring emotional impacts—each path has unique challenges.
Latest Research and Developments
The field of male infertility is always evolving, with new insights and treatments on the horizon. Let’s look at what’s new.
Emerging Treatments
-
- Stem cell therapy:
-
- Researchers are exploring ways to use stem cells to regenerate sperm-producing cells in men with NOA.
-
- Early animal studies are promising, but it’s not yet ready for clinical use.
-
- Stem cell therapy:
-
- Gene therapy:
-
- For genetic causes of azoospermia, correcting specific mutations could restore fertility.
-
- This is complex and raises ethical questions, but it’s an active area of research.
-
- Gene therapy:
-
- Artificial sperm:
-
- Scientists are working on creating functional sperm from other cells, like skin cells.
-
- While exciting, it’s still in early stages and not available for treatment.
-
- Artificial sperm:
Recent Studies
-
- A 2023 meta-analysis in the Journal of Urology found:
-
- Micro-TESE has a higher sperm retrieval rate (45-50%) than conventional TESE (25-30%) for NOA.
-
- Fresh sperm for ICSI slightly outperforms frozen sperm, though the difference is small.
-
- A 2023 meta-analysis in the Journal of Urology found:
-
- A study in the New England Journal of Medicine reported:
-
- Men with NOA who had varicocele repair before sperm retrieval had better sperm extraction rates.
-
- A study in the New England Journal of Medicine reported:
These findings highlight the importance of personalized treatment plans and the potential for ongoing research to improve outcomes.
Practical Advice for Coping and Moving Forward
Living with azoospermia takes resilience, but there are practical steps to help you navigate this journey.
Lifestyle Changes
✔️ Do:
-
- Maintain a healthy weight—obesity can affect hormone levels.
-
- Exercise regularly, but avoid overheating the testicles (e.g., hot tubs).
-
- Eat a balanced diet rich in antioxidants (fruits, veggies, nuts).
-
- Manage stress with meditation, yoga, or hobbies.
❌ Don’t:
-
- Smoke—it can harm sperm production.
-
- Drink excessively—alcohol affects hormones.
-
- Use recreational drugs—they can impair fertility.
Communication Tips
-
- With your partner:
-
- Set aside time to talk openly, using “I feel” statements.
-
- Listen actively and avoid blame.
-
- Consider couples therapy if communication is strained.
-
- With your partner:
-
- With your doctor:
-
- Write down questions before appointments.
-
- Ask for explanations in simple terms.
-
- Seek second opinions if unsure.
-
- With your doctor:
Financial Planning
Fertility treatments can be costly. Here’s how to manage:
-
- Research costs: Get estimates from clinics for procedures like IVF or micro-TESE.
-
- Check insurance: Some plans cover parts of infertility treatment—know your benefits.
-
- Explore options: Look into grants, loans, or clinical trials to offset costs.
| Treatment | Average Cost (USD) | Notes |
|---|---|---|
| IVF with ICSI | $12,000–$15,000 | Per cycle, excludes medications |
| Micro-TESE | $5,000–$10,000 | May not be covered by insurance |
| Donor sperm | $300–$1,500 | Per vial, plus insemination costs |
| Adoption | $20,000–$50,000 | Varies by agency and region |
Support Networks
-
- Online forums:
-
- Reddit’s r/infertility or FertilityIQ for community support.
-
- Share experiences and get advice from others.
-
- Online forums:
-
- Local groups:
-
- Ask your clinic or hospital about support groups for infertile couples.
-
- Attend meetings to connect face-to-face.
-
- Local groups:
Self-Care
✔️ Do:
-
- Prioritize mental health—consider therapy or counseling.
-
- Maintain hobbies—don’t let infertility consume your life.
-
- Spend time with supportive friends and family.
❌ Don’t:
-
- Isolate yourself—it can worsen depression.
-
- Neglect physical health—exercise and diet matter.
Remember, it’s okay to have good days and bad days. Be patient with yourself and your partner as you navigate this journey.
Interactive Section
To help you connect with the content, we’ve included some extras below.
Q&A with Dr. Emma Johnson, Fertility Specialist
Q: What’s the biggest misconception about azoospermia?
A: That it’s always permanent. Many men with azoospermia can still father children with the right treatment.
Q: How can couples maintain intimacy during fertility treatment?
A: Schedule date nights focused on connection, not conception. Communicate about what feels good and what doesn’t. Consider seeing a sex therapist if needed.
Q: Are there any promising new treatments?
A: Stem cell therapy shows potential, but it’s not ready for clinical use yet. For now, optimizing surgical techniques and ART protocols is key.
Knowledge Quiz
Test what you’ve learned:
-
- What does azoospermia mean?
a) Low sperm count
b) No sperm in the ejaculate
c) Poor sperm motility
- What does azoospermia mean?
-
- Which type of azoospermia might be treatable with surgery?
a) Obstructive
b) Non-obstructive
- Which type of azoospermia might be treatable with surgery?
-
- True or false: Men with azoospermia can never have biological children.
Answers: 1.b, 2.a, 3.false
Action
-
- Join our online support community: Connect with others on similar journeys.
-
- Consult a fertility specialist: Explore your specific options.
-
- Share this article: Help someone who might benefit from it.
This guide is here to support you through the challenges of azoospermia. From understanding the diagnosis to exploring treatments and coping strategies, we hope you feel empowered to take the next steps. Remember, you’re not alone, and there are paths forward—whether through medical advances, alternative family-building, or finding joy in other ways. Keep moving forward, one step at a time.


No comment