When Pieces of the Inner Lining of the Uterus Are Ectopic? A Long, In-Depth Look at Endometriosis
Introduction
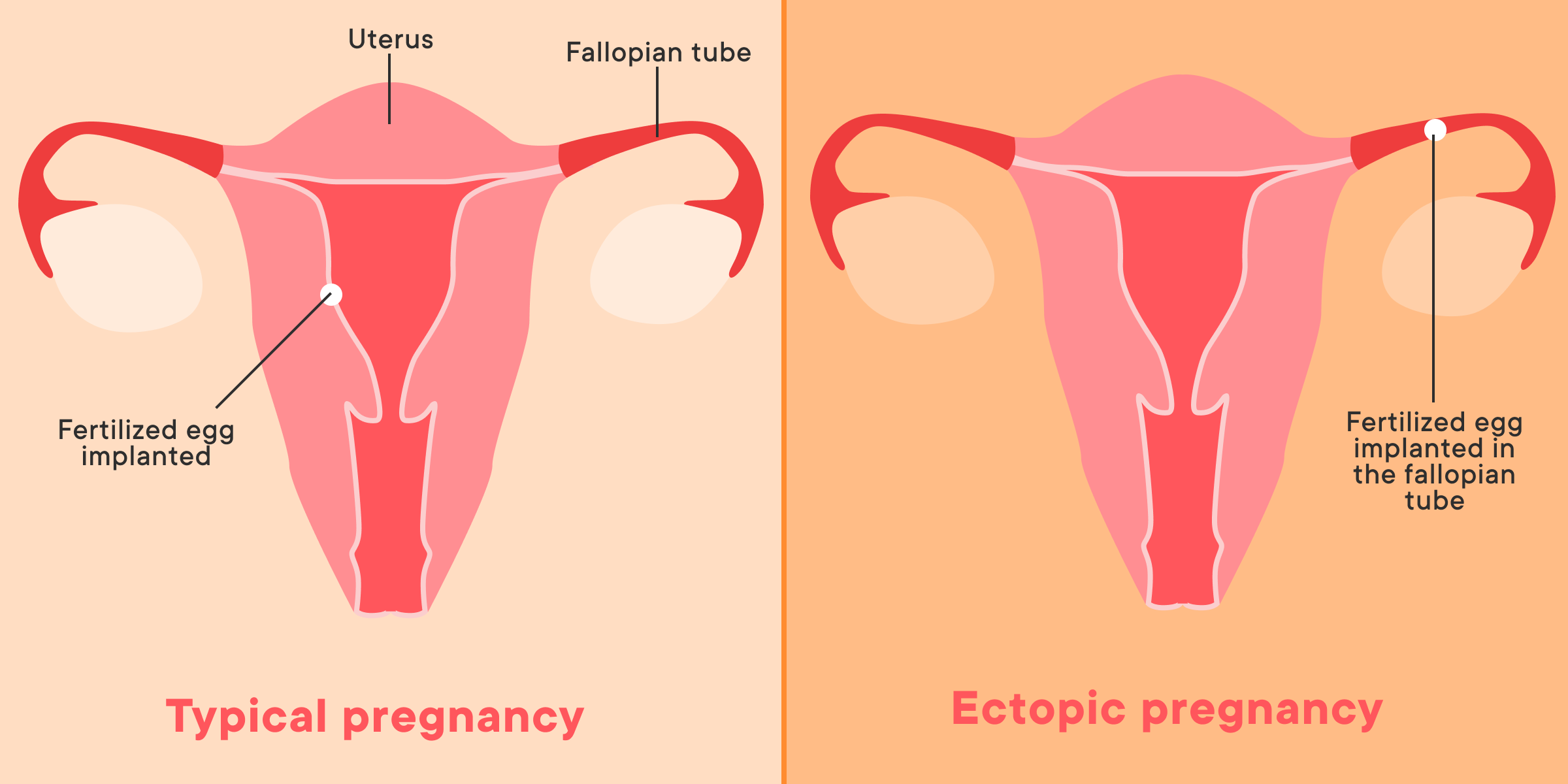
Imagine feeling pain so strong that it disrupts your everyday life—sometimes on a monthly cycle, sometimes unexpectedly. This pain might occur during your period, during sexual intercourse, or even while using the bathroom. You might suspect heavy cramps or something related to your menstrual flow, but the real cause could be deeper. This condition is often called endometriosis, which literally refers to what happens when pieces of the inner lining of the uterus are ectopic—that is, when this lining grows outside the uterus where it does not belong.
Although endometriosis is not a brand-new diagnosis, there are still many misconceptions surrounding it. In this article, you’ll find a comprehensive, reader-friendly explanation of endometriosis, including its symptoms, causes, treatment options, and practical tips for living a full, active life. We will dive deeper than most discussions, touching on rarely mentioned aspects such as the role of the gut microbiome, links to certain autoimmune features, and other less-explored areas of this disease. You’ll also find suggestions for coping with stress, lifestyle adjustments, and ideas for managing symptoms in a realistic way.
Understanding Endometriosis
What Is Endometriosis in Simple Terms?
Endometriosis happens when cells like those that usually line the inside of your uterus (endometrial cells) begin to appear elsewhere in your abdomen or pelvis. They could grow on your ovaries, fallopian tubes, or the outer walls of your uterus. In some cases, they may even appear on the bladder or bowels. Because these cells behave similarly to normal uterine lining cells, they can thicken and shed during each menstrual cycle, yet they have nowhere to go. This buildup can cause irritation, inflammation, and scarring in the areas where it grows.
Key Points:
- ✔️ Endometriosis tissue can be found on ovaries, fallopian tubes, or even abdominal organs.
- ✔️ It responds to hormonal changes, often causing cyclical pain.
- ❌ It’s not just “bad cramps.”
“Endometriosis is like an unwelcome guest that sets up a whole campsite outside the uterus and refuses to leave,” says Orion Nightingale, a reproductive endocrinologist with over 20 years of experience in women’s health.
How Common Is Endometriosis?
Studies suggest that around 10% of women of reproductive age are affected by endometriosis. Yet many individuals go undiagnosed due to lack of awareness or limited access to proper medical care. Because symptoms vary widely, a person might wait years before someone suspects endometriosis. This is why early education and awareness are critical.
The Hidden Complexities You Should Know
-
It’s Not Just a Reproductive Issue
Endometriosis can affect your day-to-day life, causing chronic pelvic pain, digestive issues, fatigue, and more. -
Can Occur Even Without Severe Cramps
Some people have mild or even no period pain yet still discover endometriosis if they undergo certain tests. -
Sometimes Overlaps with Other Conditions
There is ongoing research into links between endometriosis and migraines, autoimmune responses, and digestive disorders such as IBS. -
Possible Impact on the Gut Microbiome (Less Talked About!)
Recent studies explore how changes in gut bacteria may influence inflammation levels in people with endometriosis. While not conclusive, experts suspect that rebalancing the gut microbiome could play a role in symptom relief and overall well-being.
Recognizing Key Symptoms
Typical Symptoms
- Chronic Pelvic Pain: Pain during periods, during intercourse, or between cycles.
- Painful Periods (Dysmenorrhea): More intense cramping than usual, often accompanied by heavy bleeding or clotting.
- Irregular or Heavy Bleeding: Some people experience extended periods or spotting throughout the cycle.
- Pain During Bowel Movements: In severe cases, endometriosis growths near the bowels can cause intense pain.
Mini-Quiz: Could This Be Endometriosis?
- Do you experience pelvic pain that feels worse than regular menstrual cramps?
- Does pain disrupt your ability to work, attend school, or carry out daily tasks?
- Do you feel significant pain during or after sexual intercourse?
- Have you noticed cyclical discomfort in areas like your lower back, bladder, or bowels?
If you answered “yes” to two or more of these, you might want to discuss the possibility of endometriosis with your healthcare provider.
Less Common (But Important) Signs
- Frequent Urination: If the tissue grows near or on the bladder, it may cause urgency or a sense of incomplete emptying.
- Nausea or Digestive Problems: Symptoms like bloating, constipation, or diarrhea can be confused with other conditions, like IBS.
- Fatigue: Chronic pain and inflammation can take a toll on your energy levels.
- Infertility: Difficulty conceiving can sometimes be the first major clue.
The Unexpected Impact on Fertility
How Does Endometriosis Affect Fertility?
When endometrial tissue grows around the ovaries or fallopian tubes, it can create scar tissue that blocks or distorts these structures. This can make it more challenging for an egg to travel through the fallopian tube, reducing fertility. Even if the eggs aren’t blocked, chronic inflammation may affect egg quality or the uterine environment, making implantation harder.
Fertility Treatment Options
- Medication: Certain hormone therapies, like gonadotropin-releasing hormone (GnRH) agonists, help reduce endometriosis growth and inflammation.
- Assisted Reproductive Technology (ART): In vitro fertilization (IVF) can bypass some physical barriers caused by scarring and pelvic distortion.
- Surgical Interventions: A skilled surgeon can remove endometriosis implants or scar tissue, potentially improving fertility outcomes.
Emotional Well-Being and Mental Health
The Emotional Burden
Endometriosis isn’t just about physical discomfort. The pain can lead to emotional stress, anxiety, and sometimes depression. You might feel misunderstood by friends or even by some doctors if they minimize your symptoms.
Expert Quote 2: “Always remember that you are not defined by your illness. It’s one aspect of your life, and with the right support, you can still flourish,” says Ophelia, a therapist specializing in chronic pain.
Practical Coping Strategies
- Therapy and Support Groups: Speaking openly with mental health professionals or peers who have endometriosis can reduce feelings of isolation.
- Mindfulness and Meditation: Simple breathing exercises or guided meditations can help manage stress.
- Journaling: Keeping track of symptoms, moods, and triggers can help you and your doctor see patterns.
- Self-Compassion: Remember to be kind to yourself on days when pain sets you back.
Diagnosing Endometriosis
Initial Assessments
- Symptom History: Doctors usually begin by asking about the nature and severity of pelvic pain.
- Pelvic Exam: A manual exam can sometimes detect cysts or thickened tissue, though smaller implants may be missed.
Imaging Techniques
- Ultrasound: Helpful for spotting large cysts, but tiny deposits might not appear.
- MRI: Offers a more detailed look, but not always the first step.
Laparoscopy for a Definitive Diagnosis
Laparoscopy is a minimally invasive surgical procedure where a small camera is inserted into the abdomen to directly view the pelvic area. Doctors can see the extent of endometriosis and may remove suspicious tissue during the procedure. This step is the gold standard but usually considered after less invasive tests if symptoms strongly point to endometriosis.
Common Treatment Approaches
Medical Treatments
-
Hormone Therapy
- Birth Control Pills or Patch: Helps regulate hormones and may ease pain.
- GnRH Agonists: Temporarily reduces the body’s estrogen production.
- Mirena IUD: Releases a small, steady amount of hormone that can thin the uterine lining and reduce pain.
-
Pain Management
- NSAIDs (Nonsteroidal Anti-Inflammatory Drugs): Over-the-counter medication to reduce inflammation.
- Opioids (With Caution): Prescribed for severe pain, but come with a risk of dependence.
-
Surgery
- Laparoscopic Excision or Ablation: Removes or destroys endometriosis spots while preserving healthy tissue.
- Hysterectomy: In extreme cases, removing the uterus can be an option, though it’s not a guaranteed cure if endometriosis is also located elsewhere.
Complementary Therapies
Many people explore alternative or complementary treatments like acupuncture, herbal supplements, or nutritional therapy to ease symptoms. While these methods might not eliminate endometriosis, they can potentially improve comfort and reduce inflammation.
Taking a Holistic Approach
The Role of Diet
- Anti-Inflammatory Foods: Focus on fruits, vegetables, whole grains, and healthy fats (like avocados and nuts).
- Reduce Red Meat and Processed Foods: High levels of certain fats and additives might fuel inflammation.
- Experiment with Eliminating Triggers: Some people report fewer flare-ups after reducing gluten or dairy, although evidence is mixed.
Exercise and Physical Therapy
Gentle exercises like yoga or swimming can boost blood flow, support healthy weight, and reduce stress. In some cases, a physical therapist specializing in pelvic floor therapy can help relieve tension in the pelvic muscles.
Stress Management
- Breathing Techniques: Simple box breathing (inhaling for 4 counts, holding for 4 counts, exhaling for 4 counts, holding for 4 counts) can reduce anxiety.
- Visualization: Imagine pain or tension leaving your body with each exhale.
- Nature Walks: Spending time outdoors can improve mood and reduce stress hormones.
Three Overlooked Factors That Deserve More Attention
Here are three topics rarely discussed in mainstream articles, but important for anyone seeking a fuller understanding of endometriosis:
1. Possible Autoimmune Elements
While endometriosis is not officially classified as an autoimmune disease, there are features that look suspiciously similar to autoimmune conditions—such as elevated inflammatory markers and the body’s immune response to tissue growing where it doesn’t belong. Some studies suggest that regulating immune function might help manage symptoms.
2. The Gut Microbiome Connection
Research in 2023 highlighted that people with endometriosis often have imbalances in their gut microbiome. Although the “which causes which” question remains unsolved, improving gut health through probiotics, fermented foods, or fiber-rich diets might be beneficial. This is a developing area, so stay tuned for more data.
3. Endometriosis Beyond Menstruation
A surprising number of people with endometriosis report symptoms that persist beyond the menstrual cycle. This includes chronic fatigue, ongoing pelvic pain, and bladder discomfort. Recognizing that endometriosis can be a 24/7 condition helps shape more effective, day-to-day management strategies rather than only focusing on period pain.
Lifestyle Tips and Everyday Management
Self-Care Checklist for Endometriosis
Use this handy list to track your daily habits:
| Self-Care Item | Completed? |
|---|---|
| ✔️ Adequate Hydration (6-8 glasses/day) | |
| ✔️ 30-Minute Gentle Exercise (walk, yoga) | |
| ✔️ Anti-Inflammatory Meals | |
| ✔️ Stress-Reduction Practice (meditation) | |
| ❌ Excessive Sugar or Alcohol | |
| ❌ Skipping Sleep (aim for 7-9 hours) | |
| ❌ Overdoing High-Impact Workouts |
Filling out a checklist like this weekly or even daily can keep you consistent and help you notice which areas might need more attention.
Practical Pain-Relief Tips
- Heating Pads: Applying heat can relax muscles and improve blood flow.
- Warm Baths: This acts similarly to a heating pad but can affect a larger area of your body.
- Proper Rest: Listen to your body’s signals and rest when needed.
- Over-the-Counter Aids: Always consult a doctor before taking new medications, but NSAIDs can help reduce inflammation.
Alternative Approaches Worth Exploring
- Herbal Teas: Chamomile, ginger, and turmeric have mild anti-inflammatory properties.
- Pelvic Floor Therapy: A qualified physical therapist can teach you stretches and exercises specifically for pelvic health.
- Emotional Support Apps: If in-person support groups aren’t accessible, online communities and apps can offer real-time peer support.
In-Depth Look at the Latest Research
New Ways of Viewing the Condition
“Endometriosis used to be viewed primarily as a hormonal condition, but we now understand it has immune system components, inflammatory pathways, and possible ties to gut health,” says Caspian Sterling, a gynecologist who has contributed to recent clinical guidelines on endometriosis management.
Possible Genetic Links
Researchers are investigating specific genes that might make someone more likely to develop endometriosis. Though this science is still evolving, the idea is that certain families have a higher prevalence, suggesting a genetic predisposition.
Experimental Therapies
- Immunomodulators: Drugs that target immune system activity might one day be a solution.
- Stem Cell Research: Studies are looking at how to prevent rogue endometrial cells from developing into lesions.
- Personalized Medicine: Using genetic information and microbiome profiling to tailor individual treatment plans.
Real Stories and Personal Experiences
Why Sharing Stories Matters
Endometriosis can feel isolating. Hearing from people who’ve walked the same path can be comforting and informative. Their journeys often highlight small tips—like which foods triggered their flare-ups or which breathing exercises helped during rough days.
Poll: What’s Your Biggest Endometriosis Challenge?
-
- Pain Management
-
- Emotional Stress
-
- Finding the Right Doctor
-
- Coping with Infertility
-
- Navigating Work or School
Reflect on your answer, and consider sharing it with a close friend or support group. Bringing awareness to your personal challenges is the first step in seeking effective support.
Surgical Options and Recovery
Different Surgical Approaches
- Laparoscopic Surgery: Involves making small incisions in the abdomen to remove or burn away growths. This method is often used for both diagnosis and treatment.
- Laparotomy: A more extensive open surgery, typically reserved for severe cases or when laparoscopic tools aren’t sufficient.
- Hysterectomy: If other treatments fail and the condition severely impairs quality of life, removing the uterus might be discussed. However, endometriosis can still recur if lesions exist outside the uterus.
Tips for a Smoother Post-Surgery Recovery
- Plan for Time Off: Recovery can take several days to a few weeks, depending on the surgery.
- Stay Hydrated: Proper hydration supports healing and helps prevent constipation.
- Light Movement: Gentle walks can speed up recovery by improving blood circulation.
- Follow-Up Appointments: Regular check-ins help spot any recurring issues early.
Integrating a Long-Term Management Plan
The Role of Regular Monitoring
Endometriosis tends to be a long-term condition. Regular visits to your healthcare provider can catch new growths before they become large and symptomatic again. Adjusting medications, dietary habits, and lifestyle factors over time is often necessary.
Combining Medical and Natural Approaches
Many find that combining medical treatments with complementary methods—like specific dietary changes or yoga—offers the best balance. There’s no one-size-fits-all approach; it’s about finding what works best for you and continuously adapting.
Ongoing Support
- Support Groups: Online communities and local meet-ups can provide emotional backing.
- Professional Counseling: Chronic pain counseling can help manage stress and improve mental resilience.
- Physical Therapy: Pelvic floor specialists can be invaluable for managing pain and improving mobility.
Additional Interactive Element: Your Personal Action Plan
Below is a quick, three-step process you can follow right now:
-
Identify Your Primary Concern
Write down your top issue with endometriosis. Is it pain, fatigue, or emotional stress? -
Choose One New Strategy
Maybe you’ll add an anti-inflammatory food to your meals or start a short meditation practice. -
Set a Timeframe
Commit to trying this new strategy for at least two weeks before you assess its impact.
Using this mini-action plan can help you stay focused on small, achievable steps that build upon each other.
Looking Ahead: Hope and Future Directions
More Research, More Awareness
The number of research papers on endometriosis grows each year. More doctors are recognizing the importance of a whole-person approach that includes physical, mental, and emotional health.
Advocacy and Education
Patient advocacy groups worldwide are pushing for earlier detection, more funding for research, and better insurance coverage for treatments.
Future Possibilities
- Gene Editing: While still far off, gene-focused therapies could become an option in the future.
- Gut Microbiome Modification: We may see new targeted probiotics or dietary guidelines that specifically address the bacterial imbalances linked to endometriosis.
- Less-Invasive Diagnostics: Efforts are underway to create blood tests or other markers that can accurately identify endometriosis without the need for surgery.
Conclusion
Endometriosis is more than just a set of symptoms—it’s a complex condition that touches on physical health, emotional well-being, and even social connections. While it can disrupt everyday life, a combination of proper medical care, lifestyle adjustments, emotional support, and emerging research offers hope for better days ahead. By increasing awareness, exploring new treatments, and sharing stories, we can chip away at misunderstandings and improve the quality of life for everyone impacted by this condition.
Remember: You deserve compassionate care and real solutions, whether that’s from a trusted medical professional, online community, or a close network of friends and family. With each piece of new knowledge and each small action, you can move closer to feeling and living better—even when part of the inner lining of the uterus grows where it shouldn’t.



