Endometriosis on the Uterosacral Ligament – What You Need to Know
Endometriosis affects millions of women worldwide, yet it’s often a silent struggle that goes unnoticed or misunderstood. Imagine tissue that’s supposed to stay inside your uterus deciding to grow outside it instead—on places like your ovaries, fallopian tubes, or even a supportive band called the uterosacral ligament. When this happens on the uterosacral ligament, it’s called Uterosacral Ligament Endometriosis, and it can turn everyday activities into painful challenges.
In this article, we’re diving deep into what this condition is, how it feels, how doctors figure it out, and what you can do about it. We’ll also share real stories, expert advice, and the latest research to give you a full picture—plus some practical tips you won’t find everywhere. Whether you’re wondering if this might be you or supporting someone who’s dealing with it, we’ve got you covered with clear, friendly info you can actually use.
Let’s start with the basics.
What Is Uterosacral Ligament Endometriosis?
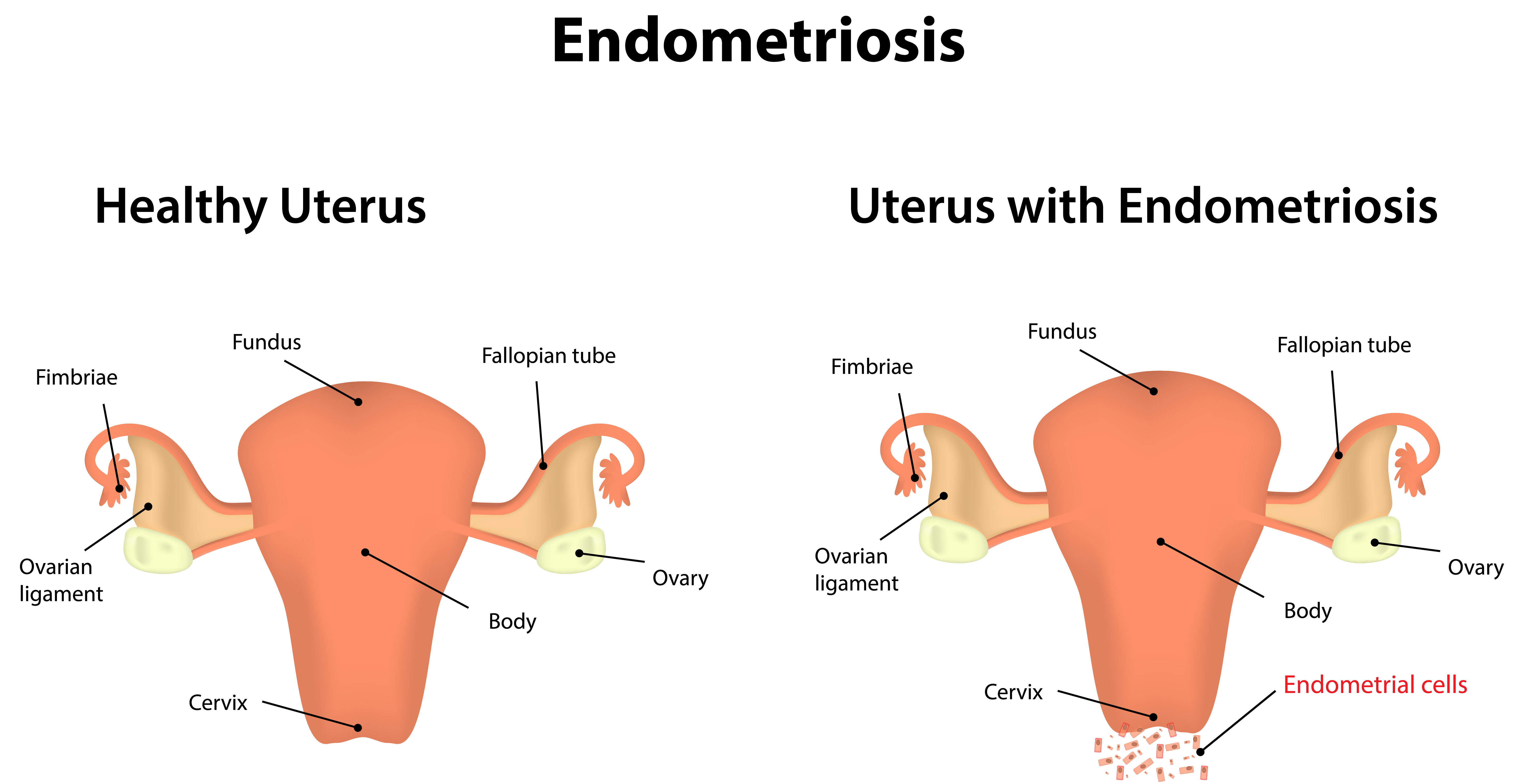
Endometriosis is when tissue similar to the lining of your uterus (the endometrium) grows where it shouldn’t—like a plant sprouting in the wrong garden. Normally, this tissue thickens and sheds each month during your period, but when it’s outside the uterus, it has nowhere to go. That’s when trouble starts.
The uterosacral ligament is a pair of strong bands that connect your uterus to the sacrum (the triangle-shaped bone at the bottom of your spine). Think of them as guy-wires holding up a tent—they keep your uterus steady, especially during pregnancy. But when endometrial-like tissue grows on these ligaments, it’s called Uterosacral Ligament Endometriosis, a type of deep infiltrating endometriosis. This means the tissue digs deep into the pelvic area, causing inflammation, scarring, and a whole lot of pain.
About 1 in 10 women of reproductive age deal with endometriosis, according to the Endometriosis Foundation of America. While we don’t know exactly how many have it specifically on the uterosacral ligament, it’s one of the most common spots for deep endometriosis to show up. Why does this happen? Experts aren’t 100% sure, but ideas include menstrual blood flowing backward into the pelvis, genetic factors, or even an immune system glitch.
Symptoms That Tell You Something’s Up
So, what does Uterosacral Ligament Endometriosis feel like? It’s different for everyone—some barely notice it, while others can hardly get out of bed. The tricky part? The pain doesn’t always match how much tissue is there. You could have a tiny bit and feel awful, or a lot and feel okay.
Here are the big signs to watch for:
-
- Pelvic Pain – A deep ache or sharp stab in your lower belly or pelvis, often worse during your period or sex. It’s like a storm brewing down there.
-
- Painful Periods (Dysmenorrhea) – Cramps that laugh at painkillers and stick around longer than they should.
-
- Pain During Sex (Dyspareunia) – Discomfort or outright pain, especially with deeper penetration, because that tissue gets irritated.
-
- Painful Pooping (Dyschezia) – If the tissue’s near your rectum, going to the bathroom during your period can hurt.
-
- Painful Peeing (Dysuria) – Same deal if it’s close to your bladder.
-
- Trouble Getting Pregnant (Infertility) – Scarring can mess with your reproductive parts, making it harder to conceive.
Then there are the sneaky extras:
-
- Feeling wiped out all the time (fatigue)
-
- Bloating that makes you feel like a balloon
-
- Nausea or upset stomach
-
- Lower back pain that won’t quit
Why does this happen? Each month, that misplaced tissue acts like it’s still in the uterus—thickening and bleeding with your cycle. But since it can’t escape, it irritates everything around it, especially those sensitive uterosacral ligaments. Some women don’t even realize they have it until they’re trying to start a family and hit roadblocks.
Could This Be You? A Quick Checklist
Wondering if this sounds familiar? Here’s a simple way to check:
-
- ✔️ Severe pelvic pain during your period?
-
- ✔️ Pain that spikes during sex?
-
- ✔️ Hurts when you poop or pee, especially around your period?
-
- ✔️ Been trying to get pregnant without luck?
If you’re nodding to any of these, it’s worth a chat with your doctor. Let’s see how they’d figure it out.
How Doctors Diagnose It
Getting a diagnosis for endometriosis isn’t a walk in the park. On average, it takes 7-10 years from when symptoms start—crazy, right? That’s because the signs can look like other problems (think IBS or ovarian cysts), and the only surefire way to know is with surgery.
Here’s how doctors typically tackle it:
1. Talking It Out and Checking You Over
Your doctor will ask about your symptoms—like when the pain hits and how bad it gets—plus your period history and if anyone in your family’s had this. Then, they’ll do a pelvic exam, feeling around for anything unusual, like tender spots or lumps on your uterosacral ligaments.
2. Peeking Inside with Imaging
These tests can’t say “yep, it’s endometriosis,” but they spot clues:
-
- Ultrasound – Uses sound waves to see cysts or growths. A transvaginal one (where they use a wand inside) is best for peeking at your pelvis.
-
- MRI – Gives a detailed map of your insides, helpful if surgery’s on the table.
3. The Big Reveal: Laparoscopy
This is the gold standard—a small surgery where a tiny camera (laparoscope) goes into your belly through a little cut. The doctor looks for that telltale tissue and might snip some out to test. Here’s what it’s like:
-
- You’re asleep with general anesthesia.
-
- They puff up your belly with gas for a better view.
-
- Tiny incisions let the camera and tools in.
-
- If they find endometriosis, they might remove it right then.
A 2022 study in the Journal of Minimally Invasive Gynecology found laparoscopy catches endometriosis missed by imaging 70% of the time—proof it’s the real deal for diagnosis.
Why It’s Tough
Symptoms overlap with other stuff, and some doctors don’t dig deep enough. That’s why picking a specialist matters—they know what to look for.
Action Step
If you’ve got symptoms and no answers, don’t give up. Ask for a referral to an endometriosis pro. Keep a symptom diary (dates, pain levels, triggers) to bring along—it’s like handing your doctor a treasure map.
Treatment Options to Feel Better
There’s no one-size-fits-all fix, but treatments can ease the pain and boost your chances of having a baby if that’s your goal. It depends on how bad it is and what you want. Here’s the lineup:
Medications: Taming the Pain
-
- Pain Relievers – Ibuprofen or naproxen for lighter days. Prescription stuff if it’s intense.
-
- Hormonal Birth Control – Pills, patches, rings, or IUDs cut menstrual flow and pain by pausing ovulation. Think of it as putting your cycle on mute.
-
- GnRH Agonists – Drugs like Lupron shrink the tissue by dropping estrogen, but they can bring hot flashes or bone thinning—like a mini-menopause.
Surgery: Cutting It Out
-
- Laparoscopic Surgery – Doctors zap or cut away the tissue, keeping your uterus intact. Great for pain and fertility.
-
- Hysterectomy – Taking out the uterus (and maybe ovaries) is a last-ditch move. It doesn’t always stop the pain if tissue’s elsewhere.
| Treatment | Pros | Cons |
|---|---|---|
| Pain Relievers | Easy, cheap | Only helps mild pain |
| Birth Control | Reduces periods, non-invasive | Side effects like mood swings |
| Surgery | Removes tissue, helps fertility | Risks, possible regrowth |
Lifestyle Hacks: Helping Yourself
-
- Move More – Exercise like walking or yoga cuts inflammation and boosts your mood.
-
- Eat Smart – Skip sugar and junk food; load up on veggies and fish. A 2021 study in Nutrients linked anti-inflammatory diets to less endo pain.
-
- Chill Out – Stress makes pain worse—try meditation or a warm bath.
What’s New?
Research is buzzing. A 2023 trial in Fertility and Sterility tested a drug targeting inflammation (not just hormones) with promising pain relief. Stay tuned!
Your Move
Talk to your doctor about mixing these—like meds plus yoga. What works for your friend might not for you, so tweak it till it fits.
The Emotional Side of Living with It
Endometriosis isn’t just physical—it can mess with your head and heart too. The pain, exhaustion, and “why me?” moments hit hard.
How It Feels
-
- Non-Stop Pain – Hard to focus at school or hang out with friends.
-
- Wiped Out – Fatigue that makes you want to nap all day.
-
- Baby Blues – Infertility stress can tank your confidence.
-
- Love Life Struggles – Painful sex can strain things with your partner.
Take Sarah, 28: “It’s like a constant ache that wears me down. I miss out on so much.” Or Emily, 32: “I feel like life’s passing me by.”
Coping Tips
-
- ✔️ Find Your People – Online groups like MyEndometriosisTeam connect you with others who get it.
-
- ✔️ Treat Yourself – Read a book, soak in a tub—small joys matter.
-
- ❌ Don’t Bottle It Up – Talk to a counselor if it’s too much.
Orion Nightingale, a gynecologist, says, “Don’t underestimate the mental toll. Support is as vital as medicine.”
Fertility Challenges and Solutions
About 30-50% of women with endometriosis struggle to get pregnant. The tissue can scar your tubes or mess with your eggs.
Options That Work
-
- Surgery – Clearing out tissue can up your odds.
-
- IVF – Eggs meet sperm in a lab, then go into your uterus—pricey but effective.
-
- Timing – Track ovulation with kits if surgery’s not your thing yet.
A 2023 Human Reproduction study showed women with deep endometriosis like this had a 40% better shot at pregnancy post-surgery. Talk to a fertility doc to map your path.
What’s Coming: Latest Research
Science is on it:
-
- Gene Clues – New markers might mean earlier tests.
-
- Immune Fixes – A 2023 Nature Reviews piece suggests immune therapies could be next.
-
- Pain Tech – Nerve blocks are in trials—less meds, more relief.
Ophelia, a women’s health researcher, shares, “We’re close to non-surgical diagnosis tools—like a blood test. It’s exciting!”
Under-the-Radar Risks and Prevention
No one’s cracked prevention yet, but risks include early periods, heavy flows, or a family history. Can’t stop it, but catching it early helps.
Watch Out For
-
- ✔️ Periods before 11? Higher odds.
-
- ❌ Skipping exercise? Might worsen inflammation.
Caspian Sterling, a pain expert, advises, “Move daily—it’s not a cure, but it lowers your risk of worse symptoms.”
Wrapping It Up
Uterosacral Ligament Endometriosis is tough, but you’ve got options—meds, surgery, lifestyle tweaks, and hope from research. Don’t wait if you suspect it; get help and take charge.
Let’s Talk About It
Quick Quiz:
-
- Period pain that’s off the charts? Yes / No
-
- Sex hurts more than it should? Yes / No
-
- Bathroom pain during your period? Yes / No
“Yes” to any? See a doc. Drop your story below—diagnosed or not, what’s worked for you? Your words could lift someone else up.
Share this if it helped!




No comment