Unlocking the Secrets of Endometrial Receptivity Testing: Your Guide to Better IVF Outcomes
Imagine you’re trying to plant a seed in your garden. You’ve got the perfect seed, but if the soil isn’t ready—too dry, too wet, or just not the right time—it won’t grow. Now think of your uterus as that garden. In fertility treatments like in vitro fertilization (IVF), your endometrium (the lining of your uterus) is the soil, and the embryo is the seed. For that embryo to take root and grow into a baby, the timing has to be just right. That’s where endometrial receptivity testing steps in—it’s like a soil test for your uterus, helping doctors figure out the exact moment your endometrium is ready to welcome an embryo.
If you’re navigating the ups and downs of IVF, you’ve probably heard about this test. Maybe you’re wondering if it could help you after months—or even years—of hoping. In this deep dive, we’ll explore everything you need to know about endometrial receptivity testing. We’ll break down what it is, how it works, who might benefit, and what the latest science says about its success. Plus, we’ll share practical tips, fresh research, and even a little interactive fun at the end to help you decide if this could be your next step toward parenthood.
What is Endometrial Receptivity Testing?
Endometrial receptivity testing is a tool doctors use during IVF to find the best time to transfer an embryo into your uterus. It checks the gene activity in your endometrial tissue to see if it’s “receptive”—meaning it’s ready for an embryo to implant and start growing.
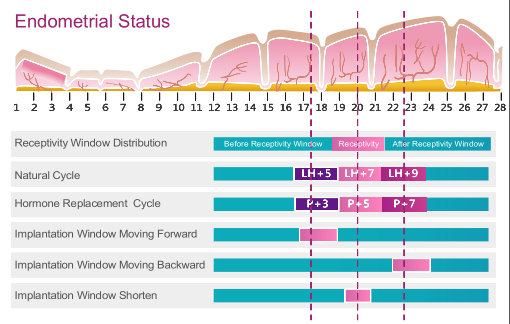
Here’s the deal: every month, your endometrium changes with your menstrual cycle, guided by hormones like estrogen and progesterone. There’s a short window—called the “window of implantation” (WOI)—when it’s perfectly primed for an embryo. For most women, this happens around days 20 to 24 of a 28-day cycle. But for some, that window might open earlier or later. Endometrial receptivity testing figures out your personal WOI, so your doctor can time the embryo transfer just right.
Think of it as a personalized calendar for your uterus. Instead of guessing when the soil is ready, this test tells you exactly when to plant that seed.
How Does Endometrial Receptivity Testing Work?
The most popular version of this test is called the Endometrial Receptivity Array (ERA). It’s a straightforward process, but it involves a few steps. Here’s how it usually goes:
-
- Getting Ready: You’ll do a “mock cycle” that mimics what happens before an embryo transfer. This means taking medications—like progesterone—to prepare your endometrium, just like you would in a real IVF cycle.
-
- Taking a Sample: At a specific point (usually when doctors think your endometrium should be receptive), a small piece of tissue is taken from your uterus. This is called a biopsy. It’s quick—think five minutes—and feels a bit like a Pap smear. Some women say it’s a little crampy, but it’s not a big deal for most.
-
- Analyzing the Genes: That tissue sample gets sent to a lab, where scientists look at 248 specific genes tied to endometrial receptivity. They compare your gene patterns to those of a “receptive” endometrium from other successful pregnancies.
-
- Getting the Results: The test tells you one of three things:
-
- Receptive: Your endometrium is ready right now—perfect timing for an embryo transfer.
-
- Pre-receptive: It’s not ready yet; you might need a couple more days of progesterone.
-
- Post-receptive: The window has already closed; you might need less time on progesterone next time.
-
- Getting the Results: The test tells you one of three things:
If your timing’s off, your doctor can tweak the plan for your next embryo transfer. It’s all about syncing up with your body’s unique rhythm.
Who Might Benefit from Endometrial Receptivity Testing?
This test isn’t for everyone going through IVF. It’s most often recommended for people who’ve hit roadblocks—like recurrent implantation failure (RIF). That’s when you’ve had several embryo transfers with healthy embryos, but they just don’t stick.
Dr. Orion Nightingale, a fertility expert, explains it this way: “For patients with RIF, endometrial receptivity testing can be a game-changer. It helps us personalize the timing of the embryo transfer, which can make all the difference in achieving a successful pregnancy.”
But RIF isn’t the only reason to consider it. Here are some other situations where it might help:
-
- Thin Endometrium: If your uterine lining struggles to thicken, this test could pinpoint whether timing is part of the problem.
-
- Donor Eggs or Embryos: When you’re using donated materials, every transfer counts, and this test might boost your odds.
-
- Limited Embryos: If you only have a few embryos left, timing them perfectly could be key.
That said, not every doctor agrees on who needs this test. Some say it’s best for tough cases, while others think it could help more people than we realize. It’s worth a chat with your doctor to see if it fits your story.
The Science Behind Endometrial Receptivity Testing
Let’s geek out for a minute. Your endometrium is amazing—it’s like a busy construction site, remodeling itself every month to get ready for a possible pregnancy. During the WOI, certain genes flip on or off, creating a sticky, welcoming surface for an embryo.
The ERA test, launched back in 2011, was a big leap forward. Before that, doctors relied on things like ultrasound (to measure thickness) or biopsies under a microscope (to check cell shapes). Those methods were okay, but they weren’t precise. The ERA uses molecular biology to look at gene activity, giving a clearer picture of receptivity.
Research backs this up—sort of. A study in the Journal of Assisted Reproduction and Genetics found that about 25% of women with RIF have a shifted WOI. When their transfer timing was adjusted after an ERA, pregnancy rates jumped. Pretty cool, right?
But here’s where it gets tricky. A big study in the New England Journal of Medicine tested ERA in a general IVF group—not just RIF patients—and found no boost in live birth rates. So, while it might be a lifesaver for some, it’s not a universal fix. Scientists are still figuring out who it helps most.
Pros and Cons of Endometrial Receptivity Testing
Every fertility tool has its upsides and downsides. Here’s a quick rundown:
Pros
-
- Custom Timing: It tailors the embryo transfer to your body, which could mean better odds of implantation.
-
- Low Risk: The biopsy is simple and safe—no major worries there.
-
- Peace of Mind: If you’ve had failures, knowing the timing is spot-on can ease some stress.
Cons
-
- Price Tag: It’s not cheap—often $600 to $1,000—and insurance might not cover it.
-
- Mixed Results: The science isn’t 100% clear on how much it helps everyone.
-
- Extra Time: You’ll need a mock cycle, which delays your real transfer by a month or so.
Dr. Ophelia, a reproductive endocrinologist, puts it this way: “Patients should weigh the costs and benefits carefully. For some, the test can be invaluable, but for others, it might not be necessary.” It’s all about what makes sense for you.
Practical Advice for Patients Considering Endometrial Receptivity Testing
Thinking about giving this test a shot? Here’s how to approach it like a pro:
-
- Chat with Your Doc: Start with a heart-to-heart about your IVF history. Have you had multiple failures? Good embryos that didn’t implant? That’s your cue to ask about this test.
-
- Know the Drill: The mock cycle and biopsy sound fancy, but they’re routine. Ask your clinic what meds you’ll take and how they’ll schedule it.
-
- Prep for the Biopsy: It’s quick, but you might feel cramps—like a strong period. Pop an ibuprofen an hour before if you’re worried. Bring a pad, too—some light spotting is normal.
-
- Decode the Results: If it says “pre-receptive” or “post-receptive,” don’t freak out. It’s just a timing tweak—like adjusting a recipe. Your doctor will explain the next steps.
-
- Check the Cost: Call your insurance to see if they’ll pitch in. If not, ask your clinic about payment plans. Some even offer discounts for bundling it with IVF.
-
- Stay Calm: This test is one piece of the puzzle. Whether it’s receptive or not, you’re still moving forward.
What’s New in Endometrial Receptivity Research?
The fertility world doesn’t stand still, and endometrial receptivity testing is getting some exciting updates. Here’s what’s bubbling up in 2023:
-
- AI-Powered Insights: A study from the European Society of Human Reproduction and Embryology (ESHRE) showed that artificial intelligence can analyze ultrasound images to predict receptivity. No biopsy needed—just a scan. It’s still early days, but it could be a game-changer.
-
- The Microbiome Factor: Your uterus isn’t sterile—it’s home to a tiny community of bacteria called the endometrial microbiome. New research hints that imbalances here might mess with implantation. A 2022 study in Fertility and Sterility found that women with certain bacterial profiles had lower receptivity. Scientists are now exploring whether probiotics or antibiotics could help.
-
- Combo Approaches: Some experts think the future is mixing tests—like gene analysis (ERA), microbiome checks, and imaging—for a fuller picture. Dr. Caspian Sterling, a reproductive medicine researcher, says, “The future of endometrial receptivity testing might lie in combining multiple approaches—gene expression, microbiome analysis, and imaging—to get a more comprehensive picture.”
These breakthroughs aren’t in clinics yet, but they’re worth keeping an eye on. They could make testing less invasive and more accurate down the road.
Common Questions Patients Ask About Endometrial Receptivity Testing
Got questions? You’re not alone. Here are the ones we hear most—and the answers to match:
Q: Does the Biopsy Hurt?
Most women say it’s more uncomfortable than painful—like a pinch or a cramp. It’s over in minutes, and any discomfort fades fast.
Q: How Accurate is the ERA Test?
The ERA is super consistent—if you test twice, you’ll likely get the same result. But whether it predicts a baby? That’s less certain. It’s a tool, not a crystal ball.
Q: Can I Do It Without Hormones?
Yes, it’s possible in a natural cycle, but most clinics use a mock hormone cycle to match your real IVF plan. Talk to your doctor about what’s best for you.
Q: What If My Results Say I’m Not Receptive?
No biggie—it just means your window is off-schedule. Your doctor will adjust your progesterone timing (more or less days) to line things up for the transfer.
Q: Will It Guarantee a Pregnancy?
Nope. It’s about improving your odds, not promising a baby. Other factors—like embryo quality—still matter.
Real Stories: How Endometrial Receptivity Testing Made a Difference
Sometimes, hearing from others helps it click. Here are two quick stories (names changed for privacy):
-
- Sarah, 34: After three failed transfers with top-grade embryos, Sarah was ready to give up. Her doctor suggested ERA, which showed her WOI was two days early. They adjusted her next transfer, and she’s now 20 weeks pregnant. “It felt like we finally cracked the code,” she says.
-
- Jen, 39: Jen had a thin endometrium and two donor egg failures. Her ERA showed she was receptive, ruling out timing issues. It didn’t lead to a pregnancy yet, but it helped her team focus on other fixes—like building her lining.
These stories show it’s not a one-size-fits-all solution, but it can be a turning point for some.
Your Step-by-Step Guide to Endometrial Receptivity Testing
Ready to dive in? Here’s a roadmap to get you through:
-
- Step 1: Ask the Question
At your next appointment, say, “Could endometrial receptivity testing help me?” Bring up your history—failed transfers, thin lining, whatever’s on your mind.
- Step 1: Ask the Question
-
- Step 2: Plan the Mock Cycle
Your clinic will set up a cycle with meds (usually estrogen and progesterone) to prep your uterus. It’s like a dress rehearsal for the real transfer.
- Step 2: Plan the Mock Cycle
-
- Step 3: Schedule the Biopsy
They’ll pick a day—often day 5 or 6 after starting progesterone—when they think you’re receptive. You’ll go in, get the biopsy (five minutes, tops), and head home.
- Step 3: Schedule the Biopsy
-
- Step 4: Wait for Results
It takes about 1-2 weeks to get the report. Use this time to rest and ask your doctor any follow-up questions.
- Step 4: Wait for Results
-
- Step 5: Adjust and Transfer
If timing’s off, your next IVF cycle gets a tweak. If it’s spot-on, you’re ready to roll with confidence.
- Step 5: Adjust and Transfer
Busting Myths About Endometrial Receptivity Testing
There’s a lot of chatter out there—let’s clear up some confusion:
-
- Myth: “It’s only for older women.”
Truth: Age doesn’t matter—it’s about implantation issues, not how old you are.
- Myth: “It’s only for older women.”
-
- Myth: “It’s super painful.”
Truth: It’s mild for most—just a quick cramp or two.
- Myth: “It’s super painful.”
-
- Myth: “It works for everyone.”
Truth: It’s most helpful for specific cases, like RIF. For others, it might not change much.
- Myth: “It works for everyone.”
Interactive Fun: Is Endometrial Receptivity Testing Right for You?
Let’s make this personal. Grab a pen or just tally in your head—here’s a quick checklist:
-
- Have you had multiple embryo transfers that didn’t work?
✔️ Yes ❌ No
- Have you had multiple embryo transfers that didn’t work?
-
- Are your embryos good quality, but they’re not implanting?
✔️ Yes ❌ No
- Are your embryos good quality, but they’re not implanting?
-
- Do you have a history of thin endometrium?
✔️ Yes ❌ No
- Do you have a history of thin endometrium?
-
- Are you using donor eggs or embryos?
✔️ Yes ❌ No
- Are you using donor eggs or embryos?
-
- Do you have just a few embryos left and want every shot to count?
✔️ Yes ❌ No
- Do you have just a few embryos left and want every shot to count?
Score It:
-
- 2 or more ✔️: This test might be worth exploring—talk to your doctor.
-
- 1 ✔️: Maybe, depending on your situation. Ask for a pro’s take.
-
- All ❌: It might not be your priority, but keep it in mind if things change.
Wrapping It Up: Your Next Move
Endometrial receptivity testing isn’t a magic wand, but for some, it’s the missing piece in the IVF puzzle. It’s about giving your embryo the best possible welcome—a perfectly timed home in your uterus. The science is still catching up, and new ideas (like AI and microbiome tweaks) are on the horizon, but for now, it’s a solid option for those who’ve hit walls.
If you’re curious, don’t sit on it. Talk to your doctor, crunch the numbers, and see if it fits your journey. You’ve got this—and whether it’s this test or another step, every move brings you closer to your goal. You’re not alone—there’s a whole community rooting for you.




No comment