Can Endometriosis Cause Pelvic Inflammatory Disease
Starting a family is a significant and joyful journey, but certain health conditions can make it more challenging. Two such conditions that often come up are endometriosis and pelvic inflammatory disease (PID). Understanding these conditions and their relationship is crucial for anyone navigating fertility and reproductive health. In this article, we’ll explore what endometriosis and PID are, whether endometriosis can cause PID, their symptoms, treatments, and tips for managing your health.
What is Endometriosis?
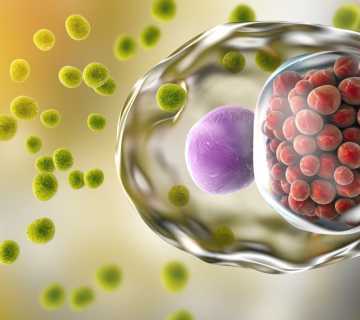
Endometriosis is a condition where tissue similar to the lining inside the uterus grows outside of it. This tissue can be found on the ovaries, fallopian tubes, and other pelvic organs. Endometriosis can cause pain, especially during menstruation, and may lead to fertility issues.
Symptoms of Endometriosis
Recognizing the symptoms of endometriosis early can help manage the condition effectively. Common symptoms include:
- Painful Periods: Severe cramps and pelvic pain during menstruation.
- Chronic Pelvic Pain: Persistent pain in the lower abdomen.
- Pain During or After Sex: Discomfort during or after intercourse.
- Pain with Bowel Movements or Urination: Especially during menstrual periods.
- Heavy Menstrual Bleeding: Excessive bleeding during periods.
- Infertility: Difficulty getting pregnant.
What is Pelvic Inflammatory Disease (PID)?
Pelvic Inflammatory Disease (PID) is an infection of the female reproductive organs. It usually occurs when sexually transmitted bacteria spread from the vagina to the uterus, fallopian tubes, or ovaries. PID can cause serious complications, including infertility, if not treated promptly.
Symptoms of PID
PID symptoms can vary but often include:
- Lower Abdominal Pain: Persistent pain in the lower belly.
- Fever: Elevated body temperature.
- Unusual Discharge: Abnormal vaginal discharge with an unusual odor.
- Pain During Sex: Discomfort during intercourse.
- Painful Urination: Burning or pain while urinating.
- Irregular Menstrual Bleeding: Spotting between periods or heavier periods.
Can Endometriosis Cause Pelvic Inflammatory Disease?
While endometriosis and PID are both conditions that affect the pelvic area, they are distinct and have different causes. Endometriosis is a chronic condition involving the growth of endometrial-like tissue outside the uterus, whereas PID is an infection caused by bacteria.
Understanding the Connection
Endometriosis does not directly cause PID, but the two conditions can influence each other in several ways:
- Inflammation: Both endometriosis and PID involve inflammation in the pelvic area. Chronic inflammation from endometriosis might make the pelvic tissues more susceptible to infections, potentially increasing the risk of PID.
- Surgical Interventions: Women with endometriosis often undergo surgeries to remove endometrial tissue. These surgical procedures can sometimes introduce bacteria, increasing the risk of PID.
- Misdiagnosis: The symptoms of endometriosis and PID can overlap, leading to misdiagnosis. If endometriosis is mistaken for PID or vice versa, appropriate treatment may be delayed, allowing the other condition to develop or worsen.
Dr. Emily Thompson, a reproductive endocrinologist, explains, “While endometriosis itself doesn’t cause PID, the overlapping symptoms and potential for increased inflammation can create a situation where the risk of PID is elevated. It’s important for women with endometriosis to be aware of the signs of PID and seek prompt medical attention if they suspect an infection.”
Causes of Endometriosis and PID
Causes of Endometriosis
The exact cause of endometriosis is unknown, but several theories exist:
- Retrograde Menstruation: Menstrual blood containing endometrial cells flows back through the fallopian tubes into the pelvic cavity instead of leaving the body.
- Genetic Factors: A family history of endometriosis increases the risk.
- Immune System Disorders: Problems with the immune system may prevent the body from recognizing and destroying endometrial-like tissue outside the uterus.
Causes of PID
PID is primarily caused by bacterial infections, often transmitted sexually:
- Sexually Transmitted Infections (STIs): Gonorrhea and chlamydia are common culprits.
- Bacterial Infections: Bacteria from the vagina or cervix can spread to the pelvic organs.
- Surgical Procedures: Gynecological surgeries or the insertion of intrauterine devices (IUDs) can introduce bacteria.
Diagnosing Endometriosis and PID
Diagnosing Endometriosis
Diagnosing endometriosis typically involves:
- Medical History and Physical Exam: Discussing symptoms and performing a pelvic exam.
- Imaging Tests: Ultrasound or MRI to identify endometrial lesions.
- Laparoscopy: A surgical procedure where a camera is inserted into the pelvic cavity to visualize and possibly biopsy endometrial tissue.
Diagnosing PID
PID diagnosis includes:
- Medical History and Physical Exam: Reviewing symptoms and performing a pelvic exam.
- Laboratory Tests: Testing for STIs through urine tests or swabs.
- Imaging Tests: Ultrasound or MRI to assess the extent of the infection.
- Laparoscopy: In some cases, a surgical procedure to view the pelvic organs directly.
Treatment Options
Treating Endometriosis
Treatment for endometriosis focuses on managing pain and improving fertility:
- Pain Relief Medications: Over-the-counter painkillers or prescription medications.
- Hormone Therapy: Birth control pills, progestins, or gonadotropin-releasing hormone (GnRH) agonists to reduce or eliminate menstruation.
- Surgical Options: Laparoscopy to remove or destroy endometrial tissue.
Treating PID
PID treatment aims to eliminate the infection and prevent complications:
- Antibiotics: A combination of antibiotics to treat the bacterial infection.
- Hospitalization: In severe cases, intravenous antibiotics and hospitalization may be necessary.
- Surgery: If abscesses form or the infection does not respond to antibiotics, surgical intervention may be required.
Dr. Sarah Williams, an infectious disease specialist, states, “Early treatment of PID is crucial to prevent long-term complications like infertility. Women should seek medical attention promptly if they experience symptoms of PID.”
Health Management Tips
Managing both endometriosis and PID involves proactive health strategies:
For Endometriosis
- Regular Exercise: Helps reduce pain and improve overall health.
- Healthy Diet: Eating a balanced diet rich in fruits, vegetables, and whole grains can help manage symptoms.
- Stress Management: Practices like yoga, meditation, or counseling can help cope with chronic pain and stress.
For PID
- Safe Sex Practices: Using condoms and having regular STI screenings can reduce the risk of PID.
- Prompt Treatment: Seeking immediate medical care for any signs of infection.
- Follow-Up Care: Ensuring that the full course of antibiotics is completed and attending follow-up appointments.
General Tips
- Regular Check-Ups: Routine visits to your healthcare provider can help catch and manage these conditions early.
- Open Communication: Talk openly with your partner and healthcare provider about any symptoms or concerns.
- Support Systems: Joining support groups or seeking counseling can provide emotional support.
Common Myths and Misconceptions
Myth 1: Endometriosis Always Causes Severe Pain
Fact: While many women with endometriosis experience significant pain, some have mild symptoms or no pain at all. The severity of symptoms can vary widely.
Myth 2: PID Only Affects Sexually Active Women
Fact: While PID is commonly associated with sexually transmitted infections, it can also occur in women who are not sexually active due to other bacterial infections or medical procedures.
Myth 3: Treating Endometriosis Will Prevent PID
Fact: Treating endometriosis focuses on managing endometrial tissue growth and pain, while PID is an infection that requires antibiotic treatment. They are separate conditions and treating one does not prevent the other.
Frequently Asked Questions
Can Endometriosis Make Me More Prone to Infections?
Endometriosis itself does not directly cause infections, but the chronic inflammation associated with it might make pelvic tissues more susceptible to bacterial infections, potentially increasing the risk of PID.
How Can I Prevent PID if I Have Endometriosis?
Practicing safe sex, getting regular STI screenings, and seeking prompt treatment for any infections can help prevent PID. Additionally, managing endometriosis effectively can reduce inflammation and overall pelvic health issues.
Is Surgery for Endometriosis Risky in Terms of Developing PID?
Surgical procedures always carry some risk of infection, including PID. However, reputable clinics follow strict sterilization and surgical protocols to minimize this risk. Discuss any concerns with your surgeon before the procedure.
Can Both Endometriosis and PID Affect My Fertility?
Yes, both conditions can impact fertility. Endometriosis can cause scarring and adhesions that affect the reproductive organs, while PID can lead to scarring of the fallopian tubes and other pelvic structures, making it difficult to conceive.
What Should I Do If I Suspect I Have Both Conditions?
If you suspect you have symptoms of both endometriosis and PID, seek medical attention immediately. A healthcare provider can perform the necessary tests to diagnose and treat each condition appropriately.
Expert Insights
Dr. Laura Martinez, a reproductive endocrinologist, emphasizes, “Understanding the differences and connections between endometriosis and PID is essential for effective treatment and maintaining reproductive health. Both conditions require timely medical intervention to prevent long-term complications.”
Dr. Michael Lee, a gynecologist, adds, “Women with endometriosis should be vigilant about any new pelvic symptoms, as the chronic inflammation can create an environment where infections like PID can thrive. Regular check-ups and open communication with your healthcare provider are key.”
Dr. Sarah Williams, an infectious disease specialist, highlights, “Early detection and treatment of PID are crucial. Women should never ignore pelvic pain or unusual symptoms, as prompt treatment can prevent serious health issues down the line.”
Conclusion
Endometriosis and pelvic inflammatory disease are two distinct conditions that affect the pelvic area, each with its own causes, symptoms, and treatments. While endometriosis does not directly cause PID, the chronic inflammation and potential for increased susceptibility to infections can create a scenario where PID is more likely. Understanding the relationship between these conditions, recognizing the symptoms, and seeking prompt medical care are essential steps in managing your reproductive health.
Remember, maintaining open communication with your healthcare provider and practicing proactive health management can significantly improve your quality of life and fertility outcomes. As Dr. Martinez wisely states, “Knowledge and early intervention are your best tools in managing both endometriosis and PID. Stay informed and take charge of your health journey.”

No comment