
IVF for PCOS Patients – Your Complete Guide
Polycystic Ovary Syndrome (PCOS) affects millions of women, making it one of the most common hormonal disorders out there. If you’re dealing with PCOS and dreaming of starting a family, you might have heard about In Vitro Fertilization (IVF) as a way to make that dream come true. But what exactly is IVF, and how does it work for someone with PCOS? This guide is here to walk you through everything you need to know—step by step, in plain language. Whether you’re just starting to explore your options or you’re ready to dive into treatment, we’ve got you covered with practical tips, the latest research, and answers to the questions you’re probably asking right now.
PCOS can feel like a roadblock when it comes to getting pregnant, but IVF offers a detour—a way to bypass some of those challenges. In this article, we’ll break down what PCOS does to your body, how IVF can help, and what you can do to boost your chances of success. We’ll also dig into stuff you might not find everywhere else, like new treatments being studied and how to handle the emotional ups and downs. Let’s get started by understanding what’s going on with PCOS and why fertility can be tricky.
Understanding PCOS and Its Impact on Fertility
Imagine your body as a big control room where hormones are the switches. In PCOS, some of those switches are flipped the wrong way. It’s a condition that messes with your ovaries—the two small organs that release eggs and make hormones like estrogen. For about 1 in 10 women, PCOS throws things off balance, leading to symptoms that can make life—and pregnancy—a little tougher.
What is PCOS?
PCOS stands for Polycystic Ovary Syndrome. The name might make you think it’s all about cysts, but it’s really about hormones. Your ovaries might have lots of tiny follicles—think of them as little sacs where eggs grow—but they don’t always release eggs like they should. This happens because your body might be making too much insulin or male hormones like testosterone. Common signs of PCOS include:
-
- Irregular periods: Maybe you skip months or get super heavy flows.
-
- Extra hair: On your face, chest, or back—places you don’t want it.
-
- Acne or oily skin: Thanks to those extra male hormones.
-
- Weight gain: Especially around your belly.
-
- Trouble getting pregnant: The big one we’re focusing on here.
Not everyone with PCOS has all these symptoms, and they can vary a lot. That’s why it’s so personal—and why figuring out your version of PCOS matters.
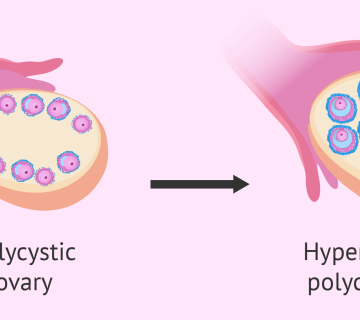
How PCOS Affects Fertility
Getting pregnant the natural way depends on ovulation—when your ovary releases an egg for sperm to fertilize. Picture it like a monthly delivery service. In PCOS, that service gets delayed or canceled. Why? The hormones that tell your ovaries to prep and release an egg are out of sync. Instead of one egg maturing, you might get a bunch of small follicles that don’t go anywhere. It’s like planting seeds that never sprout.
Then there’s insulin. Many women with PCOS have insulin resistance, meaning their bodies don’t use this sugar-controlling hormone well. Too much insulin can boost those male hormones even more, making ovulation harder. Plus, it can lead to weight gain, which adds another layer of challenge to fertility.
Other Fertility Hurdles with PCOS
Beyond ovulation, PCOS can throw in a few more curveballs:
-
- Inflammation: Some research shows that women with PCOS might have more inflammation in their bodies, which can affect egg quality.
-
- Uterine lining issues: Irregular periods can mean the lining of your uterus doesn’t build up right for an embryo to stick.
-
- Egg quality: While not always a problem, the hormonal chaos can sometimes affect how healthy your eggs are.
So, if natural conception isn’t working, what’s next? That’s where IVF steps in—a treatment that takes the process into the lab to give you a better shot.
The Four Types of PCOS—Why It Matters
Did you know there’s more than one kind of PCOS? Doctors use something called the Rotterdam criteria to identify it, and there are four main “phenotypes” based on three signs: irregular ovulation, high male hormones, and polycystic ovaries on an ultrasound. Here’s a quick rundown:
-
- Type A: All three—irregular periods, high hormones, and polycystic ovaries.
-
- Type B: Irregular periods and high hormones, but no polycystic ovaries.
-
- Type C: High hormones and polycystic ovaries, but regular periods.
-
- Type D: Irregular periods and polycystic ovaries, but normal hormone levels.
Why does this matter for IVF? Some types, like Type A, might mean a higher risk of overreacting to IVF meds, while others might respond differently. Knowing your type can help your doctor plan your treatment better. Ask your doctor to check this out—it’s a small detail that could make a big difference.
The IVF Process for Women with PCOS
IVF is like a science-powered shortcut to pregnancy. It’s a process where doctors help your eggs and sperm meet outside your body, then put the resulting embryo back inside. For women with PCOS, it’s especially helpful because it skips the ovulation problem. Let’s break it down into simple steps and see what makes it unique for you.
What is IVF?
In Vitro Fertilization means “fertilization in glass”—fancy words for doing it in a lab. Here’s the gist: Doctors take eggs from your ovaries, mix them with sperm, and grow the embryos for a few days. Then, they pick the best one (or two) and place it in your uterus to grow into a baby. For PCOS patients, IVF can be a game-changer because it doesn’t rely on your ovaries releasing eggs on their own.
Step-by-Step Guide to IVF
Step 1: Ovarian Stimulation
Think of your ovaries as a garden. Normally, they grow one “flower” (egg) a month. In IVF, doctors use meds to grow lots of flowers at once. You’ll take hormone shots—usually for 8-14 days—to boost egg production. For PCOS patients, this step needs extra care because your ovaries might go overboard, producing too many eggs. That can lead to Ovarian Hyperstimulation Syndrome (OHSS), where your ovaries swell up and hurt.
To keep this in check, doctors might use an “antagonist protocol.” This means adding a medicine to stop early ovulation and watching you closely with ultrasounds and blood tests. They might also use a special shot called a GnRH agonist trigger instead of the usual one to lower the OHSS risk.
Tips:
-
- ✔️ Ask your doctor about the antagonist protocol.
-
- ✔️ Keep a calendar for your shots—consistency is key.
-
- ❌ Don’t skip appointments; monitoring is super important.
Step 2: Egg Retrieval
Once your eggs are ready, it’s time to pick them. You’ll go to the clinic, get a light sedation so you’re comfy, and the doctor will use a thin needle to pull the eggs out through your vagina, guided by an ultrasound. It takes about 20-30 minutes, and you’ll rest for a bit before heading home.
For PCOS women, there might be more eggs to grab—sometimes 20 or more! That’s great for chances but can up the OHSS risk. Recovery tip: Rest up, drink water, and call your doctor if you feel bloated or in pain afterward.
Step 3: Fertilization
In the lab, your eggs meet the sperm. There are two ways this happens:
-
- Standard IVF: Eggs and sperm hang out together in a dish.
-
- ICSI: A sperm is injected right into each egg—handy if sperm quality is low.
For PCOS, ICSI might be used if there are tons of eggs, to make sure more get fertilized. After a day, they’ll check which ones worked and let them grow into embryos.
Step 4: Embryo Transfer
A few days later (usually 3-5), the best embryos are picked. You’ll go back to the clinic, and the doctor will slide a tiny tube through your cervix to place the embryo in your uterus. It’s quick—no sedation needed—and feels like a Pap smear. Extra embryos? They can be frozen for later.
For PCOS patients, some doctors suggest a “frozen transfer” instead of a fresh one. Why? Your body gets a break from stimulation, which might help the uterus welcome the embryo better.
Tips:
-
- ✔️ Rest after, but you don’t need to stay in bed all day.
-
- ❌ Don’t stress if you don’t feel “pregnant” right away—it’s too early to tell.
Special Considerations for PCOS
Here’s what sets PCOS apart in IVF:
-
- Higher egg count: More eggs can mean more embryos, but also more OHSS risk.
-
- Tailored meds: Your dose might be lower to avoid overstimulating.
-
- Frozen transfers: Often preferred to let your hormones settle.
Here’s a handy table to compare stimulation options:
| Protocol | What It Does | Pros | Cons |
|---|---|---|---|
| Antagonist Cycle | Stops early ovulation with a blocker | Lowers OHSS risk | Might need more meds |
| Long Protocol | Shuts down natural hormones first | Good control | Higher OHSS risk |
| Mild Stimulation | Uses less medicine | Fewer side effects | Fewer eggs |
Talk to your doctor about which fits you best!
Success Rates and Challenges of IVF in PCOS
Will IVF work for you? It’s a big question, and the answer is hopeful. Studies show that women with PCOS can have just as good a shot at pregnancy and a baby as women without it. But there are some bumps along the way. Let’s look at the numbers and how to smooth out those bumps.
Success Rates: What the Research Says
A big study from ScienceDirect found that pregnancy rates and live birth rates after IVF are similar for PCOS and non-PCOS women. That’s great news! For women under 35, the chance of a live birth per cycle can be around 40-50%, depending on the clinic and your health. PCOS doesn’t seem to lower that overall success—it’s more about managing the extras it brings.
Common Challenges and Solutions
Ovarian Hyperstimulation Syndrome (OHSS)
OHSS is the biggest worry for PCOS patients. It happens when your ovaries overreact to the meds, swelling up and leaking fluid. Mild cases might just mean bloating, but severe ones can cause pain or breathing trouble. Studies say PCOS women are about 3.5 times more likely to get OHSS.
Prevention:
-
- ✔️ Use lower med doses and the antagonist protocol.
-
- ✔️ Get a GnRH agonist trigger shot.
-
- ❌ Avoid pushing for too many eggs—quality beats quantity.
Orion Nightingale, a fertility expert, says, “For PCOS patients, the key is balance. We adjust the meds to get enough eggs without overloading the ovaries.”
Miscarriage and Early Pregnancy Loss
Research shows a slightly higher miscarriage risk with PCOS—about 1.4 times more than non-PCOS patients. Why? It might be tied to insulin issues or an uneven uterine lining from irregular cycles.
Solutions:
-
- ✔️ Manage insulin with diet or metformin before IVF.
-
- ✔️ Consider a frozen transfer to prep your uterus better.
-
- ❌ Don’t ignore pre-IVF health checks—they catch these risks early.
The Role of AMH in Predicting Success
AMH (Anti-Müllerian Hormone) is like a sneak peek at your egg supply. In PCOS, it’s often high because of all those extra follicles. A high AMH can mean you’ll get lots of eggs, but it also warns of OHSS risk. Doctors use it to pick the right med dose—too much AMH might mean a gentler approach. Ask your doctor to test yours—it’s a simple blood draw that can guide your plan.
Preparing for IVF with PCOS
IVF isn’t just about the clinic—it starts with you. Getting ready can boost your odds and make the process easier. Here’s how to prep your body and mind.
Lifestyle Changes to Boost Success
Diet
What you eat matters. PCOS loves to mess with insulin, so a diet that keeps blood sugar steady can help.
-
- ✔️ Load up on veggies, lean meats, nuts, and whole grains.
-
- ✔️ Try a low-glycemic index (GI) diet—think brown rice over white.
-
- ❌ Cut back on sugary snacks and sodas.
Sample Meal Plan:
-
- Breakfast: Oatmeal with berries and a spoonful of almond butter.
-
- Lunch: Grilled chicken salad with olive oil dressing.
-
- Dinner: Salmon, quinoa, and steamed broccoli.
Exercise
Moving your body helps insulin work better and lowers stress—two big wins for PCOS.
-
- ✔️ Aim for 30 minutes most days—walking, swimming, or yoga are great.
-
- ✔️ Mix in some strength training (like light weights) twice a week.
-
- ❌ Don’t overdo it—too much can stress your hormones more.
Weight Management
If you’re overweight, losing even 5-10% of your weight can kickstart ovulation and improve IVF results. One study found that women who dropped a little weight had better egg quality.
-
- ✔️ Set small goals—like 1-2 pounds a week.
-
- ✔️ Work with a nutritionist familiar with PCOS.
-
- ❌ Avoid crash diets—they can backfire.
Supplements and Medications
Metformin
This med helps control insulin and might improve how your ovaries respond to IVF. It’s not for everyone, but worth asking about.
Vitamin D
Lots of PCOS women are low on vitamin D, which can affect fertility. A quick blood test can tell if you need a supplement—usually 2000 IU daily does the trick.
Myo-Inositol
This natural supplement is a star for PCOS. Studies show it can improve egg quality and cut OHSS risk. Aim for 2-4 grams a day, mixed in water or as pills.
-
- ✔️ Check with your doctor before starting.
-
- ❌ Don’t mix it with random supplements—keep it simple.
Emotional Preparation
IVF can feel like a rollercoaster. Getting your head in the game is just as important as your body.
-
- ✔️ Talk to friends or join a PCOS support group online.
-
- ✔️ Try relaxation tricks like deep breathing or a warm bath.
-
- ❌ Don’t bottle up your worries—share them with someone you trust.
Caspian Sterling, a mental health expert, advises, “Take it one day at a time. Small steps—like a walk or a chat—can keep you grounded during IVF.”
Latest Research and Advancements in IVF for PCOS
Science is always moving forward, and there’s exciting stuff happening for PCOS and IVF. Here’s what’s new and what might help you.
New Techniques and Protocols
Letrozole for Stimulation
Instead of the usual meds, some doctors use Letrozole—a pill that tricks your body into making more egg-growing hormones. It’s gentler than clomiphene and might mean fewer side effects.
GnRH Agonist Triggers
This shot cuts OHSS risk big-time by changing how your eggs finish maturing. Research from 2023 backs this up for PCOS patients.
The Future of IVF
Scientists are looking at genes to figure out why PCOS happens and how to personalize IVF. Plus, AI is helping pick the healthiest embryos by analyzing pics from the lab—cool, right?
Myo-Inositol and D-Chiro-Inositol
These two supplements are hot topics. Myo-inositol helps eggs grow better, while D-chiro-inositol tackles insulin. A recent study found that a 40:1 mix of the two might boost pregnancy rates. Ophelia, a nutrition expert, says, “Getting the balance right with inositol can give your ovaries a real edge in IVF.”
Emotional and Psychological Aspects of IVF with PCOS
IVF isn’t just physical—it’s a mental marathon too. PCOS can already feel heavy, and adding fertility treatment ramps it up. Here’s how to handle it.
The Emotional Rollercoaster
You might feel excited one day, then crushed if a cycle fails. That’s normal. Common emotions include:
-
- Hope when you start.
-
- Anxiety during waiting periods.
-
- Sadness if it doesn’t work.
Coping Tips:
-
- ✔️ Write down your feelings—it’s like unloading a backpack.
-
- ✔️ Plan something fun after big steps, like a movie night.
-
- ❌ Don’t blame yourself—IVF is a team effort with your body and doctors.
Building Resilience
-
- Mindfulness: Try a 5-minute breathing exercise—inhale for 4, hold for 4, exhale for 4.
-
- Partner Talk: Share your highs and lows; it keeps you connected.
-
- Breaks: If it’s too much, pause and recharge.
Support Resources
-
- ✔️ Check out forums like Reddit’s r/PCOS or r/infertility.
-
- ✔️ Look for local fertility support groups.
-
- ❌ Don’t isolate—someone out there gets it.
Financial Considerations and Choosing a Clinic
IVF isn’t cheap, and PCOS might mean extra steps. Let’s break down the money side and how to pick a clinic.
Understanding Costs
A single IVF cycle averages $12,000-$15,000, plus $3,000-$5,000 for meds. PCOS might add costs if you need more monitoring or cycles.
-
- ✔️ Ask about package deals—some clinics bundle cycles.
-
- ✔️ Check insurance—some states cover parts of IVF.
-
- ❌ Don’t assume it’s out of reach—look into options.
Choosing a Clinic
-
- ✔️ Look at success rates for PCOS patients on the CDC’s ART site.
-
- ✔️ Ask: “How do you handle PCOS cases?”
-
- ✔️ Visit the clinic—vibes matter.
Grants and Scholarships
-
- Baby Quest Foundation: Offers grants for IVF.
-
- Starfish Infertility Foundation: Helps with treatment costs.
-
- CNY Fertility Grants: Check their site for deadlines.
Common Myths and Misconceptions About PCOS and IVF
Let’s bust some myths that might be stressing you out.
-
- Myth: “PCOS means I can’t get pregnant.”
-
- Truth: Many women with PCOS do, with or without IVF.
-
- Myth: “PCOS means I can’t get pregnant.”
-
- Myth: “IVF is my only choice.”
-
- Truth: Meds like clomiphene might work first.
-
- Myth: “IVF is my only choice.”
-
- Myth: “My eggs are all bad because of PCOS.”
-
- Truth: Quality varies—PCOS doesn’t ruin them all.
-
- Myth: “My eggs are all bad because of PCOS.”
-
- Myth: “IVF works right away.”
-
- Truth: It might take a few tries, and that’s okay.
-
- Myth: “IVF works right away.”
Conclusion
PCOS might make the road to parenthood twisty, but IVF can straighten it out. From understanding your body to prepping for treatment, you’ve got tools to take charge. With smart lifestyle tweaks, the latest science, and a solid support crew, you’re not alone on this journey. Talk to your doctor, ask questions, and keep hope alive—your story’s still being written.
Interactive Content
Quiz: Are You Ready for IVF?
Answer these to see where you stand:
-
- Have you talked to your doctor about IVF?
-
- Yes / No
-
- Have you talked to your doctor about IVF?
-
- Do you know the basic steps of IVF?
-
- Yes / No
-
- Do you know the basic steps of IVF?
-
- Have you thought about the costs and emotions?
-
- Yes / No
-
- Have you thought about the costs and emotions?
-
- Do you have people to lean on?
-
- Yes / No
-
- Do you have people to lean on?
Results: Mostly “Yes”? You’re on track! Mostly “No”? No worries—start with one step, like a doctor chat.
Checklist: Preparing for IVF with PCOS
-
- ✔️ Eat a PCOS-friendly diet for 1 month.
-
- ✔️ Start a simple exercise routine.
-
- ✔️ Ask about metformin or inositol.
- ✔️ Find a support buddy or group.



No comment