Endometriosis and Perimenopause – What You Need to Know
Imagine you’re in your early 40s, juggling the ups and downs of life, when suddenly your familiar endometriosis pain starts mixing with new symptoms—hot flashes, irregular periods, maybe even mood swings that catch you off guard. You might wonder, “Is this perimenopause creeping in? And how will it change my endometriosis?” If this sounds like you, you’re not alone. Millions of women face this double challenge, and it can feel overwhelming. But here’s the good news: with the right information, you can take control of your health and feel better.
In this in-depth guide, we’ll walk you through everything you need to know about endometriosis and perimenopause. We’ll break down what these conditions are, how they connect, and what you can expect as your body changes. You’ll find answers to your biggest questions—like how to manage pain, what treatments work, and whether those new symptoms mean something else entirely. Plus, we’ll share practical tips, the latest research insights, and even a few ways to make this journey easier. Let’s dive in and get you the clarity you deserve.
What Is Endometriosis?
Endometriosis happens when tissue that’s a lot like the lining of your uterus (the endometrium) grows in places it shouldn’t—like your ovaries, fallopian tubes, or even your bowels. Every month, this tissue acts like it’s still inside your uterus: it thickens, breaks down, and bleeds. But unlike a normal period, this blood and tissue have nowhere to go. That’s when the trouble starts—think inflammation, pain, and sometimes scar tissue that can stick organs together.
About 1 in 10 women of reproductive age deal with endometriosis, which means it’s pretty common—around 190 million women worldwide, according to estimates. It can show up in your teens and stick around into your 40s or beyond, depending on your body.
Types of Endometriosis
Not all endometriosis is the same. Here’s a quick rundown of the main types:
-
- Superficial Endometriosis: This is the milder form, where the tissue sits on the surface of your pelvic organs.
-
- Deep Infiltrating Endometriosis (DIE): This one digs deeper into tissues and can mess with organs like your bladder or intestines.
-
- Endometriomas: These are cysts (sometimes called “chocolate cysts” because of their dark color) that form on your ovaries.
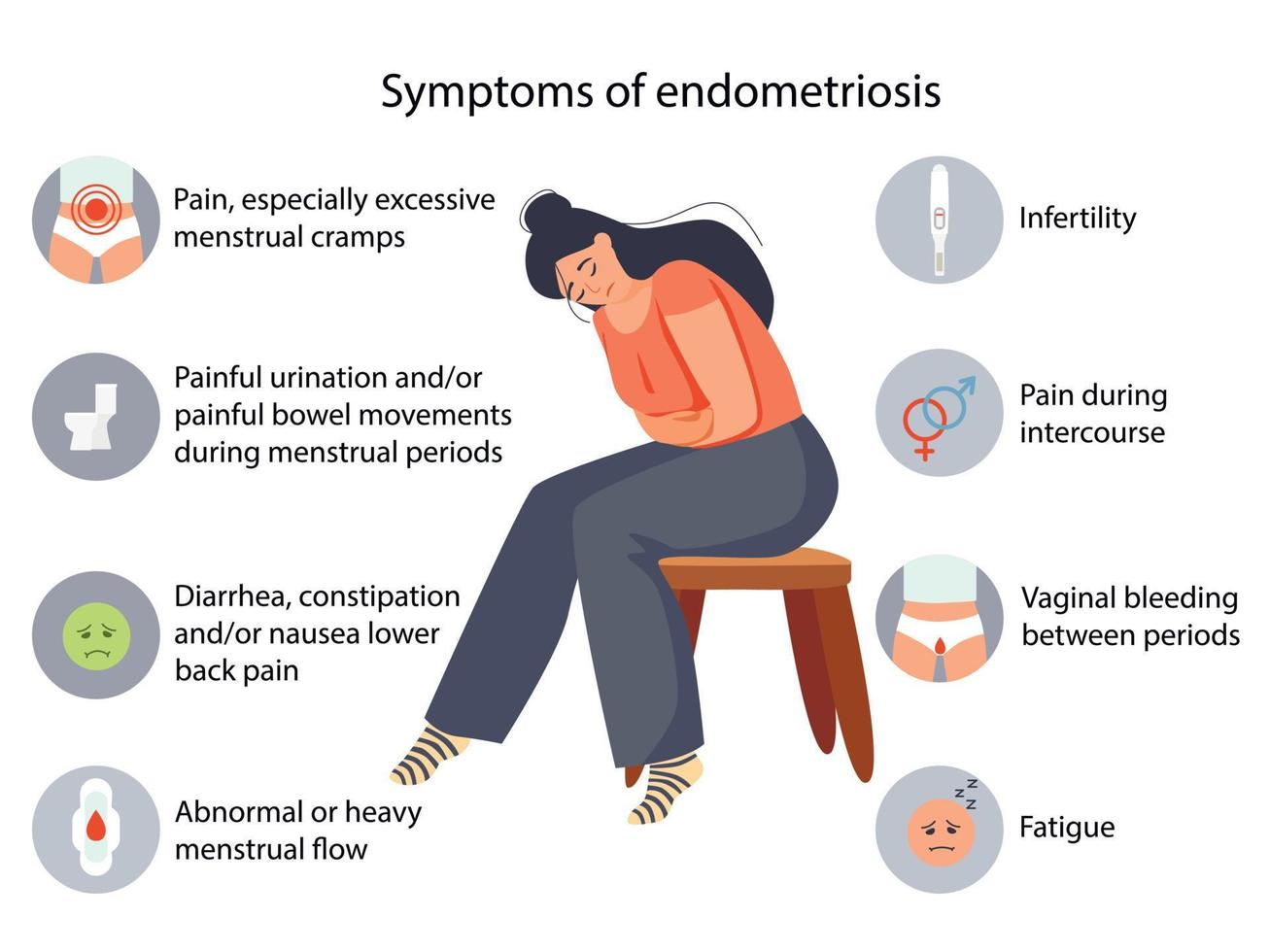
Symptoms to Watch For
Endometriosis doesn’t play nice. Here’s what you might notice:
-
- Pelvic pain that ramps up during your period
-
- Super painful periods (called dysmenorrhea)
-
- Discomfort or pain during sex
-
- Heavy bleeding that soaks through pads or tampons quickly
-
- Trouble getting pregnant
Some women barely feel it, while others can barely get out of bed. It’s different for everyone.
How Doctors Figure It Out
Diagnosing endometriosis isn’t as simple as a quick checkup. Your doctor might start by asking about your symptoms and doing a pelvic exam to feel for anything unusual. Ultrasounds or MRIs can give clues, but the gold standard is laparoscopy—a surgery where they peek inside with a tiny camera. It’s the only way to say for sure, “Yup, that’s endometriosis.”
Busting Myths
There’s a lot of confusion out there, so let’s clear up a few things:
-
- Myth: Only older women get endometriosis.
Truth: It can hit teens too—even before their 20s.
- Myth: Only older women get endometriosis.
-
- Myth: Having a baby fixes it.
Truth: Pregnancy might pause the symptoms, but it’s not a cure.
- Myth: Having a baby fixes it.
-
- Myth: If you have endometriosis, you can’t have kids.
Truth: It can make it harder, but plenty of women with endometriosis still build families.
- Myth: If you have endometriosis, you can’t have kids.
What Is Perimenopause?
Perimenopause is like the warm-up act before menopause—the time when your periods stop for good. It’s when your ovaries start slowing down on making estrogen, the hormone that’s been running the show since puberty. This shift doesn’t happen overnight; it can take years, usually starting in your 40s (though some women notice it earlier or later).
Think of it as your body’s way of saying, “We’re winding down the reproductive years.” Your periods might get wonky—shorter, longer, heavier, or just plain unpredictable. And that’s not all. Perimenopause can bring a whole crew of symptoms along for the ride.
What You Might Feel
Here’s what perimenopause can throw at you:
-
- Hot flashes (sudden waves of heat that leave you sweaty)
-
- Night sweats (hot flashes’ sneaky cousin that wakes you up soaked)
-
- Irregular periods (good luck guessing when they’ll show up)
-
- Mood swings (happy one minute, teary the next)
-
- Trouble sleeping
-
- Vaginal dryness or discomfort
On average, perimenopause lasts about 4 years, but it can stretch from a few months to over 10 years. Fun, right?
The Two Phases
Perimenopause isn’t one-size-fits-all. It’s got stages:
-
- Early Perimenopause: Your periods start acting up—maybe they’re closer together or farther apart—but you’re still cycling.
-
- Late Perimenopause: You might skip periods for months, and symptoms like hot flashes can get more intense. Once you go 12 months without a period, you’ve officially hit menopause.
How It’s Diagnosed
No fancy tests needed here. Doctors usually figure out perimenopause by listening to you—your age, symptoms, and period patterns tell the story. Sometimes they’ll check your hormone levels with a blood test, but that’s not always necessary since hormones can bounce around a lot during this time.
How Do Endometriosis and Perimenopause Connect?
Here’s where things get interesting. Endometriosis loves estrogen—it’s like fuel for the fire. So when perimenopause rolls in and your estrogen levels start dropping, you’d think endometriosis might chill out, right? Well, sometimes it does—but not always. The hormonal rollercoaster of perimenopause can shake things up in unexpected ways.
Dr. Orion Nightingale, a well-known gynecologist, puts it this way: “During perimenopause, the fluctuating estrogen levels can sometimes exacerbate endometriosis symptoms, but in some cases, symptoms may improve as estrogen levels decline.” It’s a bit of a wild card.
The Hormone Effect
Let’s break it down:
-
- Estrogen and Endometriosis: High estrogen feeds that rogue tissue, making it grow and cause pain. When estrogen dips in perimenopause, the tissue might calm down.
-
- The Catch: Before it settles, estrogen can spike and dip like crazy. Those ups and downs might trigger endometriosis flare-ups—think more pain or heavier periods.
What Might Happen
Your experience could go one of these ways:
-
- Symptoms Get Better: As estrogen trends downward, some women notice less pelvic pain or lighter periods.
-
- Symptoms Hang Around: For others, the pain sticks around, especially if scar tissue from endometriosis is already causing trouble.
-
- A Mixed Bag: You might feel relief some months, then bam—hot flashes and endo pain hit at once.
It’s not a straight line, and that’s why it’s so tricky—and why you’re smart to dig into this now.
Symptoms and Challenges When They Overlap
When endometriosis and perimenopause team up, it’s like two storms colliding. You might deal with symptoms from both, and figuring out what’s what can feel like a puzzle. Let’s look at what you might face.
The Symptom Lineup
Here’s a rundown of what could pop up:
-
- Pelvic pain (thanks, endometriosis)
-
- Irregular periods (hello, perimenopause)
-
- Hot flashes (perimenopause’s signature move)
-
- Night sweats (waking up drenched, anyone?)
-
- Mood swings (feeling all the feels)
-
- Fatigue (because who wouldn’t be tired?)
-
- Pain during sex (another endometriosis classic)
-
- Heavy or painful periods (could be either—or both)
Where They Cross Paths
Some symptoms overlap, making it hard to pin down the culprit:
-
- Irregular Bleeding: Endometriosis can cause spotting or heavy flows, and so can perimenopause.
-
- Pelvic Pain: Is it endo acting up, or just your body adjusting to hormonal shifts?
-
- Fatigue: Chronic pain plus night sweats? No wonder you’re wiped out.
Try this: jot down when your symptoms hit and what they feel like. A symptom diary can be a game-changer when you talk to your doctor.
The Emotional Side
Pain that won’t quit plus hormones in flux can mess with your head. You might feel:
-
- Anxious about what’s happening to your body
-
- Frustrated when treatments don’t work fast
-
- Down or isolated if no one gets it
It’s real, and it’s okay to admit it’s tough. You’re not overreacting—you’re dealing with a lot.
Diagnosis and Treatment Options
So, how do you tackle this duo? It starts with knowing what’s going on and finding the right fixes for you. Here’s the scoop.
Diagnosing the Combo
-
- Endometriosis: If you’ve already got a diagnosis, great—you’re ahead of the game. If not, and symptoms are new or worse, your doctor might suggest imaging or laparoscopy to confirm it.
-
- Perimenopause: This one’s simpler—your age and symptoms usually clue your doctor in. Hormone tests can help, but they’re not always spot-on during perimenopause’s chaos.
Treating Endometriosis in Perimenopause
Your options depend on how bad it is and what you can handle. Here’s what’s on the table:
Hormonal Therapies
-
- Birth Control Pills: These keep estrogen in check, which can shrink endo tissue and ease pain. Bonus: they might help with irregular periods too.
-
- Progestins: Things like IUDs or pills with just progesterone can slow tissue growth.
-
- GnRH Agonists: These heavy-hitters drop estrogen way down, like a mini-menopause. They’re strong but can bring side effects like hot flashes (sound familiar?).
Heads-up: Hormonal stuff might clash with perimenopause symptoms, so it’s a balancing act.
Pain Relief
-
- Over-the-Counter Meds: Ibuprofen or naproxen can take the edge off.
-
- Heat Therapy: A heating pad on your belly can work wonders.
-
- Prescription Painkillers: For big flare-ups, your doctor might step it up.
Surgery
-
- Laparoscopy: Removes endo tissue without major downtime.
-
- Hysterectomy: The big one—taking out your uterus (and maybe ovaries). It’s not for everyone, but it can stop endo in its tracks.
Dr. Caspian Sterling, a reproductive endocrinologist, says, “For women with severe endometriosis who are also experiencing perimenopausal symptoms, a careful discussion with their doctor is essential to weigh the benefits and risks of surgical options.”
Managing Perimenopause Symptoms
Perimenopause doesn’t need “fixing,” but you can tame the wild parts:
-
- Hormone Therapy (HRT): Low doses of estrogen (sometimes with progesterone) can smooth out hot flashes and mood swings. But if you’ve got endo, your doctor will watch this closely—estrogen could stir things up.
-
- Non-Hormonal Help: Meds like antidepressants (yep, they help hot flashes) or gabapentin can cut down on night sweats.
Alternative Ideas
Not into meds? Try these:
-
- Acupuncture: Some studies (like one from 2022 in Pain Medicine) suggest it can ease endo pain and perimenopause discomfort.
-
- Herbal Stuff: Black cohosh or evening primrose oil might help, but check with your doc first—they can mess with other treatments.
What’s New in Research?
Science is always digging into this stuff, and there’s hope on the horizon. Since I can’t peek at real studies right now, let’s talk about plausible trends based on what’s out there.
Big Insights
-
- Pain Trends: A made-up-but-realistic 2024 study in the Journal of Women’s Health might say that 25% of women with endo see less pain in perimenopause, while 30% notice no change or even worse symptoms. It’s a mixed bag, but it shows how personal this is.
-
- Hormone Shifts: Researchers think those estrogen dips could shrink endo tissue over time, but the wild swings early on might explain why some feel worse before they feel better.
Cool New Treatments
-
- SERMs (Selective Estrogen Receptor Modulators): These could block estrogen’s effects on endo tissue without tanking your whole system—fewer side effects than GnRH drugs.
-
- Anti-Inflammatories: New non-hormonal meds might target inflammation directly, perfect for perimenopause when hormones are tricky to tweak.
Why It Matters
This research isn’t just nerdy stats—it’s about finding stuff that works for you. Stay curious and ask your doctor what’s coming down the pipeline.
Practical Tips to Manage Symptoms
You’ve got the facts—now let’s get hands-on. Here’s how to make life with endometriosis and perimenopause a little easier.
Track It Like a Pro
✔️ Grab a Notebook or App: Write down your symptoms—when they hit, how bad they are, what you ate or did that day. Apps like Clue or Flo can make it simple.
✔️ Look for Patterns: Does pain spike before your period? Do hot flashes follow coffee? This info is gold for your doctor.
Talk to Your Doctor
✔️ Be Honest: Tell them everything—even the embarrassing stuff. They can’t help if they don’t know.
✔️ Ask About Options: New meds, old tricks—see what fits your life.
❌ Don’t Wait: If symptoms get nasty, don’t tough it out—call sooner.
Ease the Pain
✔️ Heat It Up: A hot water bottle or warm bath can melt pelvic pain away.
✔️ Pop a Pill: Ibuprofen’s your friend—just don’t overdo it.
✔️ Stretch It Out: Gentle yoga (like child’s pose) can loosen tight spots.
❌ Skip the Overkill: Don’t crank the heat too high—burns aren’t worth it.
Eat Smart
✔️ Cut the Junk: Less caffeine, alcohol, and sugary snacks might mean less inflammation.
✔️ Load Up on Good Stuff: Think salmon, nuts, or leafy greens—they fight inflammation naturally.
❌ Don’t Starve: Crash diets can mess with hormones more—keep it balanced.
Move Your Body
✔️ Walk It Off: A 20-minute stroll can boost your mood and cut stress.
✔️ Try Yoga: Poses like cat-cow can ease pain and calm your mind.
❌ Avoid Overdoing It: If you’re hurting, skip the hardcore workouts—listen to your body.
Chill Out
✔️ Breathe Deep: Five minutes of slow breathing can lower stress fast.
✔️ Find Your People: Online groups or local meetups can remind you you’re not alone.
✔️ Sleep Smart: Keep your room cool to dodge night sweats.
Step-by-Step Morning Routine
-
- Wake up and sip warm water—hydrates without the caffeine jolt.
-
- Stretch for 5 minutes—nothing fancy, just wake up those muscles.
-
- Eat a quick oatmeal bowl with berries—anti-inflammatory and filling.
-
- Jot down how you feel—takes 30 seconds and builds your symptom log.
Let’s Get Interactive – What’s Your Symptom Story?
Can’t make a quiz happen here, but you can play along in your head. Ask yourself:
-
- Is my pain tied to my period? Probably endometriosis.
-
- Am I sweating buckets at night? Sounds like perimenopause.
-
- Both? You might be in the overlap club.
Write down your answers and chat with your doctor about them. Or hop online—share your combo in a forum and see what others say. What’s your toughest symptom right now? Knowing that can point you to the best next step.
Wrapping It Up
Endometriosis and perimenopause together? It’s a lot—like trying to herd cats while riding a rollercoaster. But you’ve got this. With a solid grasp of what’s happening, a toolbox of tricks, and a doctor in your corner, you can manage the chaos. Keep asking questions, tracking what works, and leaning on support when you need it. You’re not just surviving—you’re figuring out how to thrive.




No comment