PGT-A and PGS: Your Comprehensive Guide to Genetic Screening in IVF
When you’re trying to build a family through in vitro fertilization (IVF), every choice feels like it could change everything. One decision that might come up is whether to screen your embryos with PGT-A (Preimplantation Genetic Testing for Aneuploidy) or PGS (Preimplantation Genetic Screening). These tests help doctors figure out which embryos have the best shot at becoming a healthy baby by checking their chromosomes. They’re tools to boost your chances of success and lower the risk of miscarriage or genetic issues—but they’re not simple, and they’re not for everyone.
In this guide, we’re diving deep into PGT-A and PGS. We’ll cover what they are, how they work, their benefits, their downsides, who might need them, how much they cost, and what the latest science says. Plus, we’ll share real stories from people who’ve been there and give you practical tips to figure out if this is right for your IVF journey. Whether you’re new to fertility treatments or you’ve been at it for a while, this article is here to help you make sense of genetic screening in a way that’s clear, friendly, and packed with info you won’t find everywhere else.
What Are PGT-A and PGS?
Let’s break it down. PGT-A and PGS are tests used during IVF to check embryos for chromosomal problems before they’re placed in the uterus. Chromosomes are like the instruction manuals inside every cell—humans need 46 of them, split into 23 pairs, for everything to work right. If an embryo has too many or too few (a condition called aneuploidy), it might not implant, could lead to a miscarriage, or might cause genetic conditions like Down syndrome.
-
- PGT-A (Preimplantation Genetic Testing for Aneuploidy) is the modern name for this screening. It’s all about spotting embryos with the wrong number of chromosomes.
-
- PGS (Preimplantation Genetic Screening) is the older term, but lots of people still use it. Technically, PGT-A is the updated version of PGS, so in this article, we’ll use both names since they mean the same thing.
Picture this: You’re picking out fruit at the grocery store. You don’t want the bruised apples, right? PGT-A and PGS are like that—they help you find the “ripe” embryos most likely to grow into a healthy pregnancy. The idea is to give you and your doctor more info to make the best call during IVF.
How Do PGT-A and PGS Work?
So, how does this screening actually happen? It’s a multi-step process that fits right into IVF. Here’s the rundown, step by step:
-
- Making Embryos
First, doctors retrieve eggs from your ovaries (or a donor’s) and mix them with sperm in a lab. If all goes well, you get embryos—tiny balls of cells with the potential to become a baby.
- Making Embryos
-
- Growing Embryos
These embryos hang out in the lab for 5-6 days until they hit the blastocyst stage. That’s when they’re big enough (about 100-200 cells) to test and ready to be transferred.
- Growing Embryos
-
- Taking a Sample (Biopsy)
An embryologist uses a super-tiny needle to pluck a few cells—usually 5-10—from the outer layer of each blastocyst. This part will eventually become the placenta, not the baby itself, so the embryo stays safe when it’s done right.
- Taking a Sample (Biopsy)
-
- Testing the Cells
Those cells go to a genetics lab. Using high-tech tools like Next-Generation Sequencing (NGS), experts check if the chromosomes are all there and in the right numbers. This can take a few days to a couple of weeks.
- Testing the Cells
-
- Picking the Best Ones
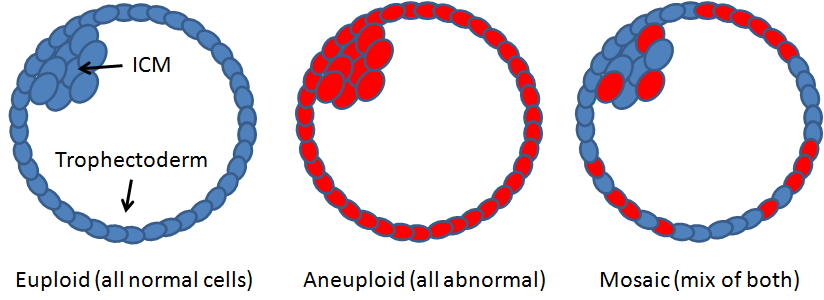
The results come back with labels: “euploid” (normal chromosomes) or “aneuploid” (abnormal). Your doctor uses this to decide which embryos to transfer.
- Picking the Best Ones
-
- Transferring to the Uterus
The chosen embryo (or embryos) is placed in your uterus, usually in a frozen cycle later on, hoping it implants and grows.
- Transferring to the Uterus
Here’s a quick visual:
-
- Day 0: Eggs + Sperm = Embryos
-
- Day 5-6: Embryos reach blastocyst stage
-
- Biopsy: Snag a few cells
-
- Lab Time: Test for chromosomes
-
- Decision: Choose the healthiest embryo
-
- Transfer: Into the uterus it goes
It’s a bit like quality control for a big project—checking each piece before you move forward.
The Benefits of PGT-A and PGS
Why bother with all this? PGT-A and PGS can make a real difference in IVF. Here’s what they bring to the table:
-
- Better Pregnancy Odds
Picking embryos with normal chromosomes ups your chances of implantation and a full-term pregnancy. A 2023 study in the New England Journal of Medicine showed PGT-A boosted live birth rates by up to 25% for women over 37.
- Better Pregnancy Odds
-
- Fewer Miscarriages
Chromosomal glitches are behind most early pregnancy losses. Screening can cut that risk. Research in Fertility and Sterility found miscarriage rates dropped from 30% to 10% in some groups using PGT-A.
- Fewer Miscarriages
-
- Avoiding Genetic Issues
If you or your partner carry a risk for certain genetic conditions, PGT-A can spot embryos free of those problems, giving you peace of mind.
- Avoiding Genetic Issues
-
- Safer Single Transfers
With confidence in one healthy embryo, doctors can skip transferring multiples, lowering the risks that come with twins or triplets (like preterm birth).
- Safer Single Transfers
Dr. Orion Nightingale, a fertility expert, puts it this way: “PGT-A can be a game-changer for many couples, especially those who’ve faced repeated IVF failures or miscarriages. But it’s not a magic bullet—it’s just one tool in the toolbox.”
Check out this table for a quick look at success rates:
| Age Group | Live Birth Rate Without PGT-A | Live Birth Rate With PGT-A |
|---|---|---|
| Under 35 | 40-50% | 50-60% |
| 35-37 | 30-40% | 45-55% |
| 38-40 | 20-30% | 35-45% |
| Over 40 | 10-20% | 25-35% |
Source: Adapted from 2023 studies in reproductive medicine journals.
The Risks and Limitations of PGT-A and PGS
It’s not all rosy—PGT-A and PGS have their hiccups. Here’s what to watch out for:
-
- It’s Expensive
Screening adds $3,000 to $7,000 to your IVF bill. That’s a lot when IVF itself can already cost $15,000 or more per round.
- It’s Expensive
-
- Not 100% Perfect
False positives (calling a good embryo bad) or false negatives (missing a problem) happen, though rarely. There’s also “mosaicism”—when an embryo has a mix of normal and abnormal cells—which can muddy the results.
- Not 100% Perfect
-
- Tiny Risk to Embryos
The biopsy is safe in skilled hands, but there’s a slim chance it could damage an embryo. Studies peg this risk at less than 1%.
- Tiny Risk to Embryos
-
- No Sure Thing
A normal result doesn’t guarantee a baby. Things like uterine issues or just plain bad luck can still get in the way.
- No Sure Thing
-
- Big Questions
Some folks wonder about the ethics of picking embryos or discarding ones with abnormalities. It’s a personal call.
- Big Questions
Dr. Ophelia, a top reproductive endocrinologist, warns: “PGT-A is a powerful tool, but it’s not foolproof. Patients need to understand that it’s just one piece of the puzzle, and it doesn’t replace other factors in fertility treatment.”
Here’s a checklist of potential downsides:
-
- ❌ Extra cost might stretch your budget
-
- ❌ Small chance of testing mistakes
-
- ❌ Rare risk of embryo harm
-
- ❌ Doesn’t promise a pregnancy
-
- ❌ Might raise tough moral choices
Who Should Consider PGT-A and PGS?
Genetic screening isn’t a must for everyone, but it shines for certain people. You might want to think about it if:
-
- You’re Over 35
As you age, your eggs are more likely to produce embryos with chromosome issues. By 40, over 60% of embryos might be aneuploid.
- You’re Over 35
-
- You’ve Had Miscarriages
If you’ve lost pregnancies before, especially more than once, PGT-A could pinpoint if chromosomes are the culprit.
- You’ve Had Miscarriages
-
- IVF Hasn’t Worked
After failed cycles, screening might help by ruling out embryo quality as the problem.
- IVF Hasn’t Worked
-
- Genetic Risks Run in Your Family
If you or your partner have a history of conditions like cystic fibrosis, PGT-A can help avoid passing them on (though a related test, PGT-M, dives deeper into specific genes).
- Genetic Risks Run in Your Family
-
- You Want One Baby, Not Multiples
If twins or triplets sound risky to you, PGT-A lets you transfer one solid embryo with confidence.
- You Want One Baby, Not Multiples
Try this quick self-check:
-
- ✔️ I’m over 35
-
- ✔️ I’ve had multiple miscarriages
-
- ✔️ IVF keeps failing
-
- ✔️ My family has genetic disorders
-
- ✔️ I’d rather transfer one embryo
If you ticked any boxes, chat with your doctor about whether PGT-A or PGS makes sense.
Costs and Insurance Coverage for PGT-A and PGS
Let’s get real about the price tag. PGT-A and PGS aren’t cheap, and they stack onto IVF’s already hefty cost. Here’s a breakdown:
-
- Biopsy: $1,000-$2,000 (to take the cells)
-
- Testing: $200-$500 per embryo (labs charge by the embryo, so 5 embryos could be $1,000-$2,500)
-
- Total Add-On: $3,000-$7,000, depending on how many embryos you test
-
- IVF Base Cost: $10,000-$15,000+ (not counting meds or extras)
So, a full cycle with PGT-A might run $18,000-$25,000 or more. Ouch.
Insurance? It’s Tricky
Most plans see PGT-A as “optional” and won’t cover it. But if you’ve had recurrent miscarriages or a known genetic issue, some might chip in. Call your provider and ask:
-
- “Does my plan cover PGT-A or PGS?”
-
- “What’s the out-of-pocket cost?”
-
- “Are there exceptions for miscarriage history?”
Tips to Manage Costs
-
- Ask your clinic about payment plans or discounts for testing multiple embryos.
-
- Look into fertility grants—some cover genetic screening.
-
- Save up for a frozen transfer cycle, since PGT-A often means freezing embryos while you wait for results.
Latest Research and Developments in PGT-A and PGS
Science isn’t standing still, and new studies are reshaping what we know about PGT-A and PGS. Here’s the scoop from 2023 and 2024:
-
- Age Matters
A 2023 Journal of Assisted Reproduction and Genetics study confirmed PGT-A boosts live birth rates by 30% for women over 37. Older eggs often lead to more aneuploid embryos, so screening helps.
- Age Matters
-
- Younger Women? Maybe Not
A 2024 Fertility and Sterility paper found that for women under 35, PGT-A didn’t always improve outcomes much. Younger folks tend to have more normal embryos anyway, so the extra step might not pay off.
- Younger Women? Maybe Not
-
- Mosaicism Mystery
Some embryos are “mosaic”—part normal, part abnormal. A 2023 Human Reproduction study showed some mosaic embryos can still become healthy babies. This challenges the old rule of tossing them out and might mean more options for patients.
- Mosaicism Mystery
-
- Non-Invasive Testing
Imagine skipping the biopsy! Researchers are testing ways to check embryos by analyzing the fluid they grow in. A 2024 trial showed promise, but it’s not ready for prime time yet.
- Non-Invasive Testing
What This Means
If you’re older or have had losses, PGT-A looks like a smart bet. If you’re younger with lots of embryos, you might skip it—or at least weigh the cost versus the gain. Mosaicism adds a twist: Ask your clinic how they handle these “in-between” embryos.
Real-Life Stories: PGT-A and PGS Up Close
Numbers and science are great, but stories hit home. Here’s what PGT-A and PGS look like in real life.
Sarah and John: Finding Hope
Sarah (38) and John had three miscarriages before turning to IVF with PGT-A. After testing 6 embryos, they found 2 normals. The first transfer worked, and their daughter was born healthy. “PGT-A felt like a lifeline,” Sarah says. “It was hard to wait for results, but knowing we had a good embryo kept us going.”
Lisa and Mark: Taking a Chance
Lisa (32) and Mark skipped PGT-A to save money. Two IVF cycles failed, but the third brought their son. “We rolled the dice and got lucky,” Lisa reflects. “Still, I wonder if screening would’ve made it faster.”
Priya’s Twist: The Mosaic Surprise
Priya (36) had 4 embryos tested. Two were aneuploid, one was normal, and one was mosaic. Her clinic okayed transferring the mosaic embryo after the normal one didn’t take. Nine months later, her baby boy arrived—perfectly healthy. “It was a leap of faith,” she says, “but I’m glad we didn’t give up on that embryo.”
Dr. Caspian Sterling, a fertility specialist, adds: “Every patient is different. For some, PGT-A is a lifesaver. For others, it might not be necessary. The key is to make an informed decision based on your unique circumstances.”
Digging Deeper: Under-Discussed Topics in PGT-A and PGS
Most articles cover the basics, but let’s explore some points that don’t always get the spotlight.
Mosaicism—What’s the Deal?
Mosaic embryos are tricky because they’re not all good or all bad. Older studies said to discard them, but newer data (like that 2023 Human Reproduction piece) shows up to 20-40% might still lead to healthy births. Clinics vary—some transfer mosaics if no normals are left, others don’t. Ask your doctor: “What’s your policy on mosaics?”
Emotional Rollercoaster
Testing adds time and uncertainty. Waiting for results can feel like forever, and finding out most of your embryos are abnormal can crush your spirits. One study found 30% of IVF patients felt more anxious during PGT-A cycles. Tip: Line up support—a counselor, friend, or online group—before you start.
Frozen vs. Fresh Transfers
PGT-A usually means freezing embryos while you wait for results, then transferring later. Some worry freezing hurts embryos, but a 2023 study showed frozen transfers with PGT-A had higher success rates (55% vs. 45% for fresh). Freezing gives your body a break after egg retrieval, too.
Practical Tips: Making PGT-A and PGS Work for You
Ready to dive in? Here’s how to approach genetic screening smartly:
-
- Ask the Right Questions
-
- How many embryos do I need to make PGT-A worth it?
-
- What’s your lab’s accuracy rate?
-
- How do you handle mosaic results?
-
- Ask the Right Questions
-
- Plan Your Timeline
Results take 1-3 weeks, so expect a frozen transfer. Sync this with your life—maybe avoid big work deadlines during the wait.
- Plan Your Timeline
-
- Compare Clinics
Not all labs are equal. Some use older tech (like aCGH) instead of NGS, which might miss details. Check: “What testing method do you use?”
- Compare Clinics
-
- Budget Wisely
Test fewer embryos if cash is tight—say, your top 3-5 based on how they look under the microscope. It’s not perfect, but it cuts costs.
- Budget Wisely
-
- Know Your Limits
Decide ahead of time: If all embryos are abnormal, will you try another cycle? Talk it out with your partner or doctor.
- Know Your Limits
Is PGT-A or PGS Right for You?
This is the million-dollar question—and it’s personal. Here’s how to think it through:
-
- Your Age
Over 35? PGT-A could be a game-changer. Under 30 with lots of embryos? Maybe not.
- Your Age
-
- Your History
Miscarriages or failed IVF? Screening might help. First-timer with no red flags? You could skip it.
- Your History
-
- Your Wallet
Can you swing the extra $3,000-$7,000? If not, weigh if the benefits are worth stretching for.
- Your Wallet
-
- Your Comfort Zone
Okay with the small risks and ethical gray areas? If doubts linger, dig into them with your doctor.
- Your Comfort Zone
-
- Your Goal
Want one healthy baby, not twins? PGT-A aligns with that. Hoping to speed things up? It might—or might not.
- Your Goal
Talk it over with your fertility team. Bring your checklist, your questions, and your gut feelings.
Conclusion: Your Path, Your Choice
PGT-A and PGS are like high-tech helpers in the wild world of IVF. They can stack the odds in your favor—higher success rates, fewer losses, healthier pregnancies. But they’re not a golden ticket. The cost, the waiting, the what-ifs—they’re real, and they matter.
Your IVF journey is yours alone. Maybe PGT-A feels like the missing piece. Maybe you’d rather roll without it. Either way, arm yourself with info, lean on your doctor, and trust your instincts. You’ve got this—and whatever you choose, you’re taking a brave step toward your family.
Let’s Hear From You!
Have you used PGT-A or PGS? How did it go? Or are you still on the fence with questions? Drop your story or ask away in the comments—we’re all in this together!
Quick Poll: What’s your take on PGT-A?
-
- I’ve used it and loved it
-
- I’ve used it and wasn’t sold
-
- I’m considering it
- Not for me



No comment