Cleavage vs. Blastocyst – Which Embryo Transfer Stage Is Right for You?
When you’re going through in vitro fertilization (IVF), one of the biggest decisions you’ll face is when to transfer your embryo into the uterus. Should it happen at the cleavage stage, around day 3, or should you wait until the blastocyst stage, around day 5 or 6? This choice isn’t just a technical detail—it can directly affect your odds of holding a baby in your arms. It’s a hot topic among fertility doctors and patients alike, and for good reason: the stakes are high, and the science is fascinating.
In this deep dive, we’ll break down everything you need to know about growing embryos to the cleavage or blastocyst stage. We’ll explore what these stages mean, weigh their pros and cons, look at the latest success rates, and unpack the factors that might sway your decision. Plus, we’ll share practical tips, answer common questions, and spotlight cutting-edge research that could shape your IVF journey. Whether you’re new to IVF or a veteran looking for clarity, this guide will arm you with the knowledge to talk confidently with your doctor.
Understanding Embryo Development Stages
Embryos don’t just magically turn into babies—they grow through distinct stages, and timing is everything in IVF. Let’s walk through the basics of how an embryo develops after fertilization.
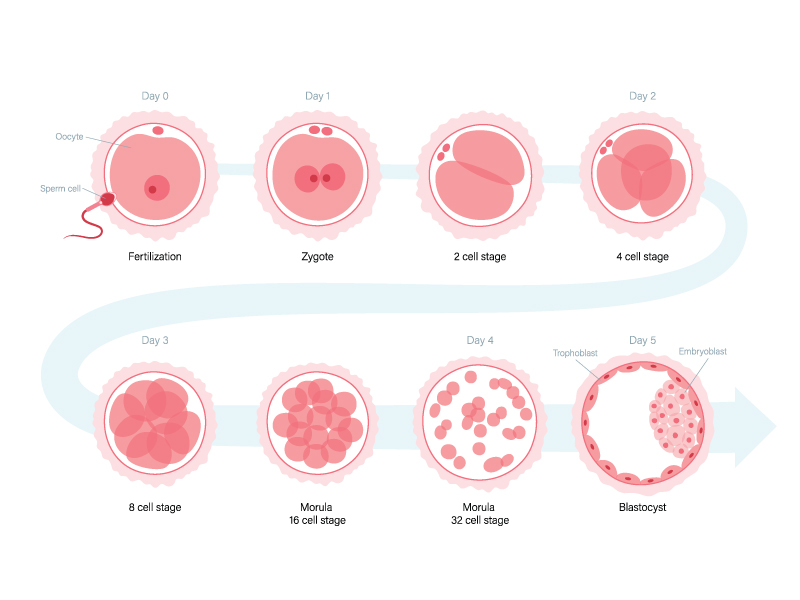
After an egg meets sperm, it starts dividing into more cells. Here’s the timeline in simple terms:
-
- Day 1: The fertilized egg, called a zygote, has two genetic starter packs—one from each parent.
-
- Day 2: It splits into 2 to 4 cells.
-
- Day 3: Now at 4 to 16 cells, it hits the cleavage stage.
-
- Day 4: The cells compact into a ball called a morula.
-
- Day 5-6: It becomes a blastocyst, with 60 to 100 cells and specialized parts forming.
Back in the day, doctors usually transferred embryos at the cleavage stage because labs couldn’t keep them growing longer. But today, thanks to better technology, many clinics can grow embryos to the blastocyst stage—which has sparked a big debate about what’s best.
What’s the Cleavage Stage All About?
Picture the cleavage stage as an embryo’s toddler years. By day 3, it’s got 4 to 16 cells, all pretty much the same—like a tiny pile of building blocks that haven’t decided what they’ll become yet. Transferring at this stage used to be the go-to move in IVF, and it’s still common for some patients.
What Happens at the Blastocyst Stage?
Fast forward to day 5 or 6, and the embryo’s a blastocyst. Now it’s more like a teenager—bigger, with 60 to 100 cells, and starting to figure itself out. It has two parts: an inner cell mass (the future baby) and an outer layer called the trophectoderm (the future placenta). This is closer to what naturally lands in the uterus during a regular pregnancy, which is why some experts love it.
Pros and Cons of Each Transfer Stage
So, which stage is better for transferring your embryo? It depends. Both cleavage and blastocyst transfers have upsides and downsides. Let’s break them down.
Cleavage Stage Transfer
✔️ Pros:
-
- Lab-friendly: Growing embryos to day 3 is a breeze for most IVF clinics.
-
- Great for fewer embryos: If you’ve only got a couple of embryos, moving them to the uterus early means less risk of losing them if they don’t grow further in the lab.
-
- Less chance of cancellation: You’re not waiting as long, so there’s a lower risk of a cycle crashing because no embryos survive.
❌ Cons:
-
- Lower success rates: The numbers show cleavage-stage embryos don’t implant or lead to live births as often as blastocysts.
-
- More embryos needed: To boost your odds, doctors might transfer two or more, which could mean twins or triplets (cute, but risky).
Blastocyst Stage Transfer
✔️ Pros:
-
- Better success rates: Blastocysts are about 1.5 times more likely to result in a live birth—pretty impressive!
-
- Natural selection at work: Only the strongest embryos make it to day 5 or 6, so you’re picking the champs.
-
- Single embryo option: Higher success means doctors often transfer just one, cutting the chance of multiples.
❌ Cons:
-
- Survival of the fittest: Some embryos might not make it to blastocyst in the lab, even if they could’ve worked in the uterus earlier.
-
- Lab skills matter: Not every clinic can grow blastocysts well—you need a top-notch team.
-
- Not for everyone: If you’re older or have few embryos, waiting might not be the best call.
Fertility expert Orion Nightingale puts it this way: “For patients with a solid batch of embryos, waiting for the blastocyst stage can really boost your chances. But it’s not a magic bullet—it’s got to fit your situation.”
Success Rates and Hard Numbers
Numbers don’t lie, and they’re a big reason blastocyst transfers are gaining fans. Let’s look at the data.
A study of over 1,600 IVF patients across 15 trials found that blastocyst transfers had a live birth rate of about 45%, compared to 30% for cleavage-stage transfers. That’s nearly 1.5 times better odds! Implantation rates—the percentage of embryos that stick in the uterus—tell a similar story: 40% for blastocysts versus 25% for cleavage-stage embryos.
Plus, blastocysts shine in single embryo transfers. In the U.S., about 80% of elective single transfers use blastocysts, showing how much confidence doctors have in them. Why? Stronger embryos mean less need to roll the dice with multiples.
Here’s a quick snapshot:
| Metric | Cleavage Stage | Blastocyst Stage |
|---|---|---|
| Live Birth Rate | 30% | 45% |
| Implantation Rate | 25% | 40% |
| Single Embryo Transfers | Less Common | ~80% of Cases |
But here’s the catch: these stats aren’t one-size-fits-all. Your age, embryo quality, and clinic’s track record can shift the odds.
What Influences the Decision?
Choosing between cleavage and blastocyst isn’t a coin flip—it’s a puzzle with pieces like these:
-
- Your Age: Younger women (under 35) often have more embryos and better blastocyst success. Older patients might lean toward cleavage transfers to play it safe.
-
- Embryo Count: Got a bunch? Waiting for blastocysts lets you pick the best. Just a few? Cleavage might be smarter to avoid losing them.
-
- Past IVF Rounds: If cleavage transfers didn’t work before, blastocyst could be a fresh shot.
-
- Genetic Testing: Planning preimplantation genetic testing (PGT-A)? Blastocysts are the safer bet—taking cells at this stage does less harm.
-
- Clinic Skill: Some labs are blastocyst wizards; others aren’t. Ask about their “blastocyst conversion rate”—aim for 40% or higher.
Fertility specialist Ophelia says, “Genetic testing is way safer and more spot-on with blastocysts. If you’re thinking PGT-A, talk to your doctor about going to day 5 or 6.”
Latest Research and Tech Breakthroughs
IVF isn’t stuck in the past—new discoveries are shaking things up. Here’s what’s hot:
-
- Genetic Testing Edge: Research shows testing blastocysts for genetic issues (like Down syndrome) barely dents their implantation rates, unlike cleavage-stage testing. It’s a game-changer for families wanting healthy pregnancies.
-
- Better Culture Media: Labs now use souped-up liquids that mimic a womb better, helping more embryos reach blastocyst stage.
-
- Time-Lapse Imaging: This cool tech lets embryologists watch embryos grow 24/7 without opening the incubator. It’s like a baby monitor for your embryos, spotting the strongest ones for transfer.
Embryologist Caspian Sterling raves, “Time-lapse imaging is changing the game. It gives us a front-row seat to embryo development, especially at the blastocyst stage.”
Practical Tips for Your IVF Journey
Facing this decision can feel overwhelming, but you’ve got this. Here’s how to tackle it:
-
- Talk to Your Doctor: Ask, “Based on my age and embryos, what’s your take?” Get personal advice, not just stats.
-
- Check Your Clinic’s Chops: Ask, “What’s your blastocyst conversion rate?” A solid clinic hits 40% or more.
-
- Weigh Risks vs. Rewards: Blastocysts might mean higher success, but also a chance of fewer embryos to transfer.
-
- Think Money and Mindset: Extra lab days for blastocysts could cost more and test your patience—be ready.
-
- Ask About Testing: If genetic screening’s on the table, lean toward blastocysts for safety.
Your Top Questions, Answered
Got questions buzzing in your head? Here are answers to what patients ask most:
Will My Embryos Reach Blastocyst Stage?
About half of fertilized eggs make it to blastocyst, but it’s not a sure thing. Quality at day 3 and your clinic’s skills play a big role.
Does Blastocyst Transfer Cost More?
Sometimes, yes—extra lab time can add fees. Call your clinic and get the scoop.
Can Cleavage Embryos Be Tested Genetically?
It’s doable but dicier than testing blastocysts. Most pros say wait for day 5 or 6.
What If I Don’t Have Many Embryos?
With just a few, cleavage transfer might be safer—no one wants to risk a total loss.
Does Transfer Stage Affect Baby’s Health?
So far, studies say no—babies from both stages seem equally healthy. More research is coming, though.
Wrapping It Up
Deciding between cleavage and blastocyst transfer is a big moment in your IVF story. Blastocysts often lead with higher success rates and smarter embryo picks, but cleavage transfers have their place, especially if you’re working with fewer embryos or a less advanced lab. Your age, embryo stash, and clinic’s expertise all tip the scales.
The best move? Team up with your doctor. Armed with this info—pros, cons, stats, and all—you can ask sharp questions and find what fits you. IVF’s a marathon, not a sprint, and this choice is one step toward your finish line.
Your IVF Decision Checklist
Ready to chat with your doctor? Take this checklist along:
-
- ✔️ What’s your clinic’s blastocyst conversion rate?
-
- ✔️ Which stage fits my age and embryo quality?
-
- ✔️ Any extra costs for blastocyst culture?
-
- ✔️ Risks of waiting if I have few embryos?
-
- ✔️ Genetic testing—doable, and when?
-
- ✔️ Success rates for patients like me?
Jot down the answers and feel more in control of your next steps.




No comment