Navigating the IVF Journey – Steps, Decisions, and What You Need to Know
Imagine you’re about to plant a garden, but the soil needs a little extra help to grow something amazing. That’s kind of what IVF, or In Vitro Fertilization, is like—a way to give nature a boost when starting a family feels out of reach. If you’re here, you might be curious, hopeful, or even a bit nervous about what lies ahead. Don’t worry—we’re going to walk through every step of the IVF process together, unravel the decisions you’ll face, and sprinkle in some fresh insights to make it all feel less intimidating. This isn’t just a science lesson; it’s your roadmap to understanding IVF, packed with practical tips, real examples, and answers to questions you didn’t even know you had.
Let’s dive into this journey, step by step, so you can feel prepared and empowered.
What Is IVF? A Simple Breakdown
IVF is a medical process that helps people have a baby when getting pregnant naturally isn’t happening. Here’s the basic idea: doctors take an egg from a woman’s body, pair it with sperm in a lab, and then place the resulting embryo back into the uterus to grow. It’s like matchmaking for cells, with a little lab magic thrown in. About 1 in 6 couples face fertility challenges, according to the CDC, and IVF has helped millions worldwide—over 8 million babies have been born this way since it started in 1978!
Why does this matter? Because IVF isn’t just one quick step—it’s a series of stages, each with choices that can shape your experience. Knowing what’s coming can turn a confusing process into something you feel ready to tackle.
The IVF Process – Your Step-by-Step Guide
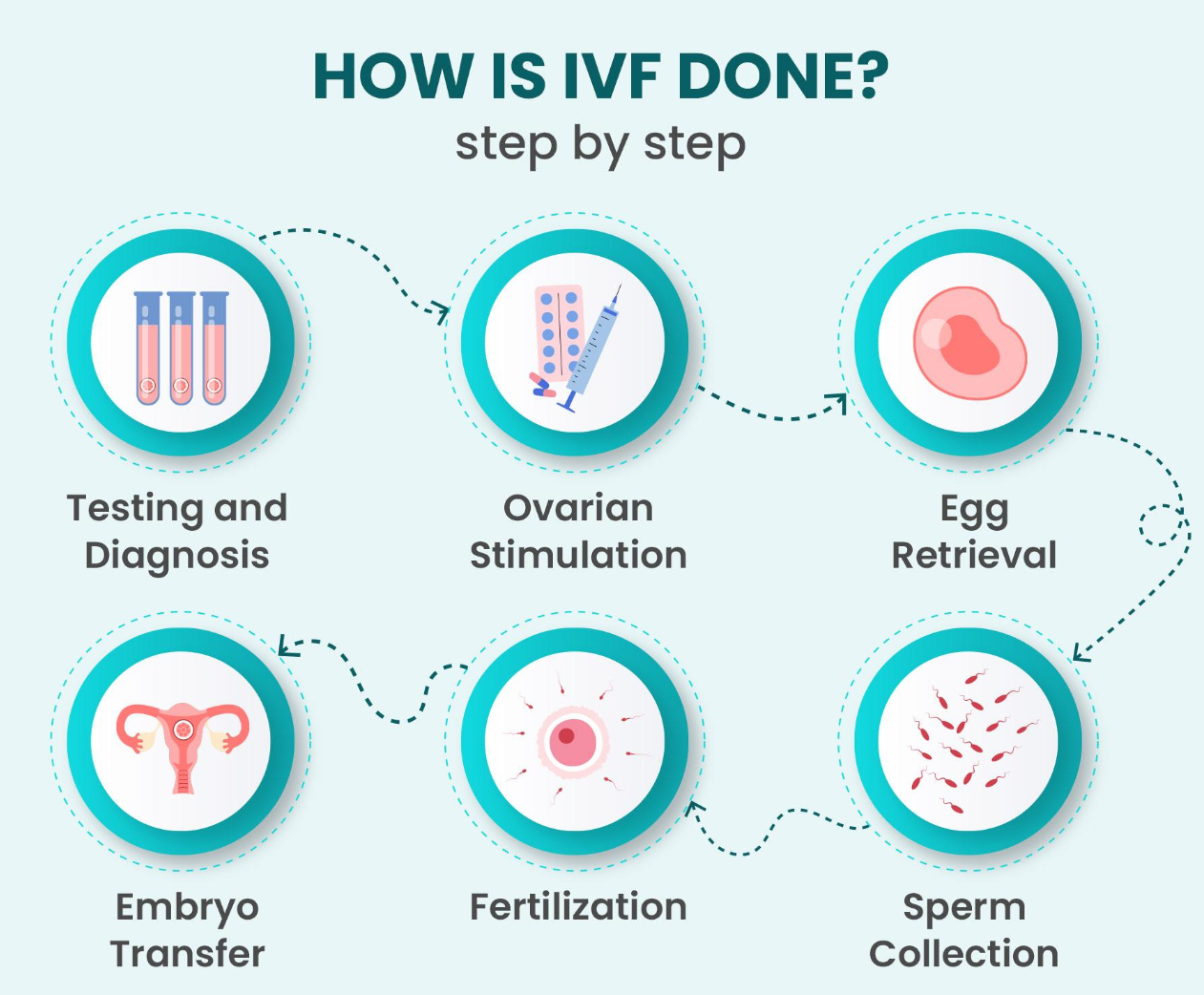
Here’s a quick look at the six main steps of IVF. We’ll dig deeper into each one soon, but this is your bird’s-eye view:
-
- Ovarian Stimulation – Boosting your ovaries to make more eggs.
-
- Egg Retrieval – Collecting those eggs for the lab.
-
- Fertilization – Mixing eggs and sperm to create embryos.
-
- Embryo Culture – Growing the embryos until they’re ready.
-
- Embryo Transfer – Placing the embryo(s) into your uterus.
-
- The Two-Week Wait – Waiting to see if you’re pregnant.
Think of these steps like chapters in a book—each one builds on the last, and your decisions help write the story.
Step 1: Ovarian Stimulation – Revving Up Your Ovaries
What’s Going On?
Your body usually releases one egg a month, but IVF needs more to work with. You’ll take hormone medications (usually shots you give yourself) to encourage your ovaries to produce several eggs at once. This lasts about 10-14 days, with regular doctor visits to check your progress using ultrasounds and blood tests.
Key Decisions
-
- Which Meds to Use?
There are options like FSH (Follicle-Stimulating Hormone) or a combo of drugs. Your doctor picks based on your age, health, and fertility history.
- Which Meds to Use?
-
- How Much Medication?
Too little might mean fewer eggs; too much could lead to Ovarian Hyperstimulation Syndrome (OHSS), where your ovaries overreact—think bloating or discomfort. About 1-2% of IVF patients experience severe OHSS, per a 2022 study in Fertility and Sterility.
- How Much Medication?
Science Says
A 2023 study from the American Society for Reproductive Medicine found that personalized dosing (tailored to your body) can increase egg yield by 20% without raising risks. It’s all about balance.
Practical Tips
✔️ Stick to the Schedule – Set phone reminders for shots.
✔️ Ask for Help – If needles freak you out, have a partner or friend assist.
❌ Don’t Skip Check-Ups – Missing an ultrasound could mess up timing.
Expert Insight: “Choosing the right dose is like tuning a guitar,” says Dr. Orion Nightingale, a fertility specialist. “Too tight or too loose, and the music’s off. We aim for harmony.”
Step 2: Egg Retrieval – Harvesting the Goods
What’s Going On?
When your eggs are ripe, a doctor collects them in a 15-20-minute procedure. You’ll be sedated, and they’ll use a thin needle guided by ultrasound to pull the eggs from your ovaries. It’s quick and painless while you’re out.
Key Decisions
-
- When to Pull the Trigger?
A “trigger shot” (like hCG) tells your ovaries to release the eggs. Timing this shot—usually 36 hours before retrieval—is critical.
- When to Pull the Trigger?
-
- Sedation Level
Light sedation is common, but some opt for full anesthesia if they’re extra nervous.
- Sedation Level
Science Says
A 2021 review in Human Reproduction showed that precise trigger timing boosts egg quality by up to 15%. Miss it, and the eggs might not be ready.
Practical Tips
✔️ Rest Up Post-Procedure – Take it easy for a day; mild cramping is normal.
✔️ Hydrate – Water helps your body recover.
❌ Don’t Stress the Numbers – You might get 5-20 eggs—every body’s different.
Pro Tip: “Egg retrieval is like picking the best fruit at the market,” says Nurse Ophelia. “You want them just right—not too early, not too late.”
Step 3: Fertilization – Where the Magic Starts
What’s Going On?
In the lab, your eggs meet the sperm. There are two ways this happens:
-
- Standard IVF – Eggs and sperm mingle in a dish, letting nature take its course.
-
- ICSI – A single sperm is injected into each egg, often used if sperm quality is low.
Key Decisions
-
- IVF or ICSI?
ICSI costs more (about $1,500 extra) but can double success rates if sperm struggles, per a 2022 Journal of Assisted Reproduction study.
- IVF or ICSI?
-
- Whose Sperm?
Partner’s or donor? Fresh or frozen? These choices depend on your situation.
- Whose Sperm?
Science Says
ICSI now accounts for 70% of IVF cycles globally, according to the European Society of Human Reproduction—proof it’s a game-changer for many.
Practical Tips
✔️ Talk Sperm Options Early – Don’t wait until the last minute to decide.
✔️ Freeze a Backup – If using a partner’s sperm, a frozen sample avoids stress on retrieval day.
❌ Don’t Assume One Way Fits All – What worked for a friend might not suit you.
Step 4: Embryo Culture – Growing Tiny Possibilities
What’s Going On?
Fertilized eggs become embryos and grow in an incubator for 3-6 days. The lab watches them, picking the strongest ones for transfer.
Key Decisions
-
- Day 3 or Day 5 Transfer?
Day 5 embryos (blastocysts) have a 5-10% higher success rate, says a 2023 Reproductive BioMedicine Online report, but fewer embryos survive that long.
- Day 3 or Day 5 Transfer?
-
- Test or Not?
Preimplantation Genetic Testing (PGT) checks for issues like Down syndrome. It’s optional and costs $3,000-$5,000.
- Test or Not?
Science Says
PGT can cut miscarriage rates by 30% in women over 35, per a 2022 study in Nature Medicine. It’s not for everyone, but it’s a powerful tool.
Practical Tips
✔️ Ask About Embryo Grading – Labs score embryos (e.g., 4AA is top-notch).
✔️ Discuss Freezing Extras – Leftover embryos can be saved for later.
❌ Don’t Obsess Over Numbers – Quality beats quantity here.
Step 5: Embryo Transfer – Planting the Seed
What’s Going On?
The doctor slides a tiny tube through your cervix to place one or two embryos in your uterus. It’s fast—no anesthesia needed—and you’re awake.
Key Decisions
-
- How Many Embryos?
One reduces twin risks (10-15% chance with two); two ups pregnancy odds but complicates things.
- How Many Embryos?
-
- Fresh or Frozen?
Frozen transfers are surging—60% of U.S. cycles in 2023—because they let your body recover first.
- Fresh or Frozen?
Science Says
A 2023 Lancet study found frozen transfers have a 7% higher live birth rate for women with high hormone levels post-retrieval.
Practical Tips
✔️ Relax Beforehand – A full bladder helps the doctor see better.
✔️ Plan a Chill Day – Rest, but no bed rest is required.
❌ Don’t Panic Over Twinges – Mild sensations are normal.
Expert Insight: “Transfer is like setting a kite aloft,” says Dr. Caspian Sterling, an embryologist. “You’ve done the work; now let it soar.”
Step 6: The Two-Week Wait – Holding Your Breath
What’s Going On?
You wait 10-14 days to see if the embryo sticks. You might take progesterone to help your uterus, then test for pregnancy.
Key Decisions
-
- How Active to Be?
Light activity is fine; heavy lifting isn’t.
- How Active to Be?
-
- When to Test?
Blood tests at the clinic are more accurate than home kits.
- When to Test?
Science Says
Stress doesn’t ruin IVF odds, per a 2021 Psychology Today review, but staying calm helps you feel better.
Practical Tips
✔️ Distract Yourself – Binge a show or start a hobby.
✔️ Lean on Support – Chat with friends or a counselor.
❌ Don’t Test Too Early – False negatives happen before day 10.
Top IVF Questions Answered
Let’s tackle what’s on your mind—because IVF sparks a lot of curiosity.
How Much Does IVF Cost?
One cycle averages $15,000 in the U.S., but it ranges from $10,000 to $20,000 depending on meds and extras like ICSI. Insurance might cover some; 19 states mandate it partially.
What Are My Chances?
For women under 35, about 33% of cycles lead to a baby, per 2022 CDC data. Over 40, it drops to 10%. Age matters most.
Is IVF Safe?
Mostly, yes. Risks like OHSS (1-2%) or ectopic pregnancy (2-5%) exist but are rare with good care.
What If It Fails?
Half of first cycles don’t work. You can tweak the plan—new meds, frozen embryos—or take a break. A 2023 survey found 70% of couples try again.
Bonus Insight – The Emotional Side of IVF
Google’s top articles often skip this, but IVF isn’t just physical. It’s a rollercoaster—hope one day, worry the next. A 2022 Journal of Fertility Counseling study found 40% of IVF patients feel anxious during the process. Here’s how to cope:
-
- Journal It – Write down highs and lows.
-
- Set Small Goals – Celebrate each step, not just the end.
-
- Find Your Tribe – Online forums like Reddit’s r/infertility can connect you with others.
Your IVF Action Plan – A Handy Checklist
Ready to start? Use this to stay on track:
✔️ Pick a clinic with solid reviews and success rates.
✔️ Book your first consult—bring questions!
✔️ Get tested (hormones, sperm, etc.).
✔️ Start meds and nail the schedule.
✔️ Prep for retrieval—rest up after.
✔️ Decide on embryos (how many, when).
✔️ Survive the wait with distractions.
✔️ Test day—fingers crossed!
Final Thoughts – You’ve Got This
IVF is a big deal, but it’s also a chance—a shot at something incredible. You’ll make choices, face surprises, and learn a ton about yourself along the way. Over 300,000 IVF cycles happen yearly in the U.S. alone, so you’re in good company. Take it one step at a time, ask for help when you need it, and know that every decision brings you closer to your goal.
Got a question or story to share? Drop it in the comments—we’d love to hear from you!




No comment