Navigating IVF with Polycystic Ovaries: A Complete Guide
Polycystic Ovary Syndrome (PCOS) affects millions of women worldwide, often making the dream of starting a family feel out of reach. If you’re one of the many women dealing with PCOS and struggling to conceive, you’ve probably heard about In Vitro Fertilization (IVF) as a possible solution. But what does IVF really mean for someone with polycystic ovaries? How does it work, and what can you do to make it a success?
This isn’t just another basic overview. We’ve dug deep into the latest research, looked at what people are searching for, and pulled together a guide that’s more thorough, more practical, and more tailored to your needs than anything else out there. Whether you’re just curious about IVF or ready to take the plunge, this article will walk you through everything—step-by-step, in a way that’s easy to understand and packed with real, actionable advice.
Let’s get started on this journey together.
Understanding PCOS: What It Is and Why It Matters
PCOS can feel like a mystery, even to those living with it. To make sense of how IVF fits in, we first need to unpack what PCOS is, how it’s spotted, and why it messes with fertility.
What Exactly is PCOS?
PCOS is a hormonal condition that throws your body out of balance. Your ovaries, which are supposed to release an egg each month, start acting up. They might produce too many male hormones (called androgens), form tiny cysts (like a string of pearls on an ultrasound), or stop ovulating regularly. This trio of trouble can lead to symptoms like:
-
- Irregular periods—maybe they’re late, super heavy, or don’t show up at all
-
- Extra hair growth on your face, chest, or back (hirsutism)
-
- Stubborn acne or oily skin that won’t quit
-
- Weight gain, especially around your midsection
-
- Hair thinning on your scalp
-
- Dark skin patches, often under your arms or on your neck
Not everyone with PCOS has all these signs, and the mix can differ from person to person. That’s part of what makes it tricky.
How Doctors Diagnose PCOS
Figuring out if you have PCOS isn’t as simple as one test. Doctors use something called the Rotterdam criteria, which means you need two out of these three things:
-
- Irregular or missing periods—a sign your ovaries aren’t releasing eggs (anovulation)
-
- High androgen levels—either shown in a blood test or through symptoms like excess hair
-
- Polycystic ovaries—lots of small follicles (not true cysts) seen on an ultrasound
Here’s a twist: you don’t actually need cysts to have PCOS, despite the name. Confusing, right? It’s more about the hormonal chaos than the cysts themselves.
Why PCOS Makes Getting Pregnant Harder
Fertility starts with ovulation—when your ovary releases an egg for sperm to fertilize. With PCOS, that process gets stuck. If your hormones are out of whack, your eggs might not mature or release on schedule. No egg, no pregnancy. It’s like waiting for a bus that never shows up.
Plus, many women with PCOS deal with insulin resistance, where your body doesn’t use insulin well. This can mess with egg quality and make it tougher for a fertilized egg to settle into your uterus. About 70% of women with PCOS face fertility challenges, making it the top reason for anovulatory infertility.
But here’s the good news: IVF can step in where nature stalls.
IVF Explained: How It Helps Women with PCOS
IVF might sound intimidating, but it’s a lifeline for many women with PCOS. Let’s break it down into simple terms and see why it’s such a powerful option.
What is IVF?
IVF stands for In Vitro Fertilization, a process where doctors help you get pregnant by doing some of the work outside your body. “In vitro” means “in glass,” like in a lab dish. Here’s the gist:
-
- Eggs are taken from your ovaries
-
- They’re fertilized with sperm in a lab
-
- The resulting embryos are placed into your uterus
It’s like giving nature a nudge when things aren’t working on their own.
Why IVF Works Well for PCOS
For women with PCOS, the biggest roadblock is ovulation—or the lack of it. IVF skips that problem entirely. Instead of waiting for your ovaries to cooperate, doctors stimulate them to produce multiple eggs, collect them, and take over from there. It’s a workaround that can turn a frustrating situation into a hopeful one.
Plus, women with PCOS often have a lot of eggs waiting in the wings (those follicles on the ultrasound). With the right care, that can mean more chances to create healthy embryos.
What Makes IVF Different for PCOS Patients?
While the IVF steps are similar for everyone, PCOS adds a few twists:
-
- More eggs, more possibilities: Your ovaries might churn out 15-20 eggs in one cycle, compared to 8-12 for others. That’s a bonus, but it needs careful handling.
-
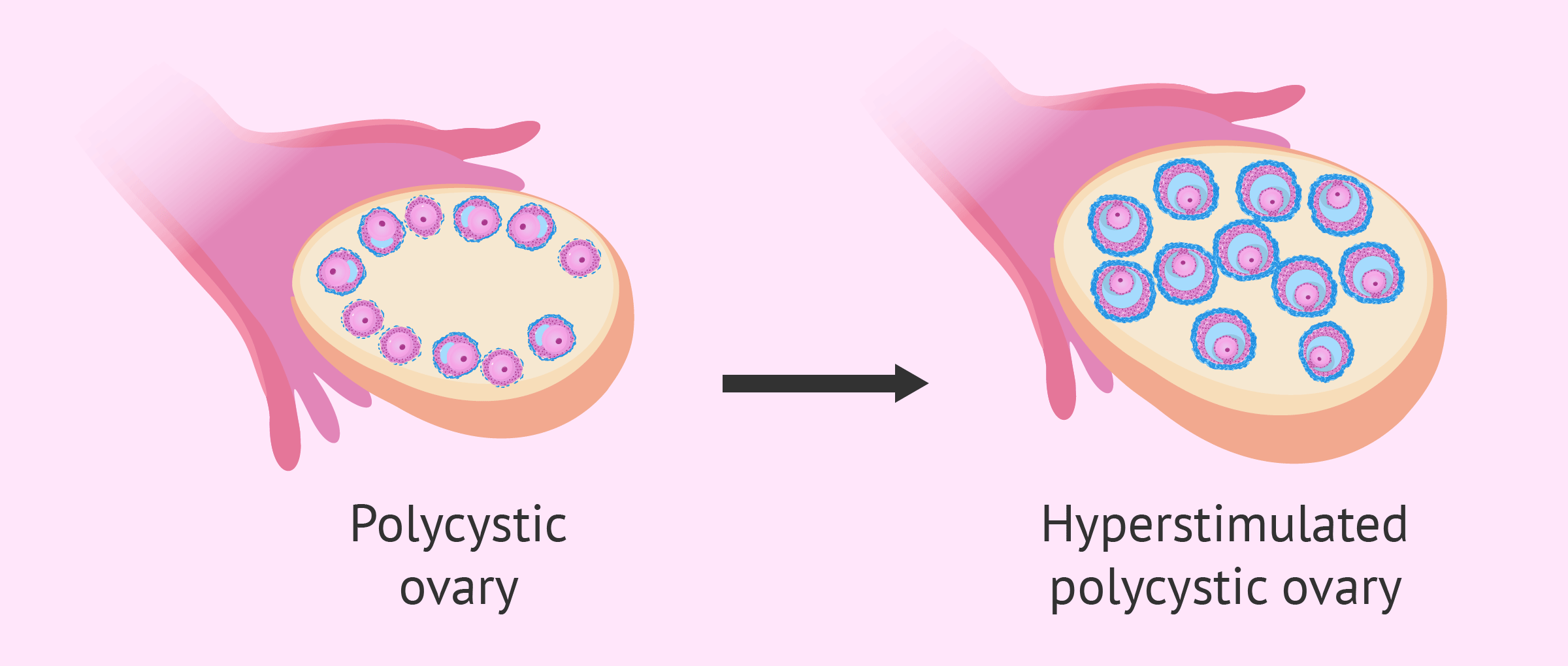
- Higher risk of OHSS: Ovarian Hyperstimulation Syndrome (OHSS) is when your ovaries overreact to meds, causing swelling or discomfort. It’s more common in PCOS because of all those eager follicles.
-
- Egg quality watch: Quantity doesn’t always mean quality. Hormonal imbalances can sometimes lead to eggs that don’t fertilize as well.
Don’t let that scare you—doctors have ways to manage these quirks, and we’ll dive into those later.
Preparing for IVF: Setting Yourself Up for Success
IVF isn’t just about what happens in the clinic. How you prepare can shape your experience and your odds of success. For women with PCOS, this prep work is extra important.
Lifestyle Changes That Make a Difference
Your daily habits can have a huge impact on IVF. Here’s what you can do:
-
- Get to a healthy weight: Extra pounds can worsen PCOS symptoms and lower IVF success. Losing just 5-10% of your body weight (say, 10 pounds if you’re 200) can kickstart ovulation and improve your chances.
-
- Eat smart: Load up on veggies, fruits, lean meats, and whole grains. Cut back on sugary snacks and processed junk—they spike insulin and throw hormones off.
-
- Move your body: Aim for 30 minutes of exercise most days—walking, swimming, or dancing all count. It helps with weight and insulin resistance.
-
- Chill out: Stress can mess with your hormones even more. Try deep breathing, yoga, or a relaxing hobby.
✔️ Quick Checklist for Pre-IVF Lifestyle Tweaks:
-
- Drink water instead of soda
-
- Swap fries for a side salad
-
- Take a 20-minute walk after dinner
-
- Set aside 10 minutes to unwind each day
Medications and Supplements to Consider
Your doctor might suggest meds or supplements to get your body IVF-ready:
-
- Metformin: This diabetes drug helps with insulin resistance, improving egg quality and cutting OHSS risk. Studies show it can boost pregnancy rates by up to 20% in PCOS patients.
-
- Clomid or Letrozole: Sometimes used before IVF to regulate cycles or test ovulation.
-
- Gonadotropins: These are the big guns during IVF, stimulating your ovaries to make eggs.
Supplements Worth a Look:
-
- Myo-inositol: A natural compound that mimics insulin’s effects. Research from 2022 found it improved egg quality in 60% of PCOS women during IVF.
-
- Vitamin D: Low levels are common in PCOS and linked to poorer fertility. A simple blood test can check yours.
-
- Omega-3s: Found in fish oil, these reduce inflammation and support hormone balance.
❌ Heads-Up: Don’t start supplements without your doctor’s OK—they can interact with IVF drugs.
Mental Prep: Why It Matters
IVF can be an emotional rollercoaster. The waiting, the uncertainty, the hope—it’s a lot. For women with PCOS, who might already feel worn out from fertility struggles, mental health is a game-changer.
-
- Find your people: Join an online PCOS or IVF group. Hearing “I get it” from someone who’s been there can lift a huge weight.
-
- Talk it out: A therapist who knows fertility issues can teach you coping tricks.
-
- Treat yourself: Carve out time for things you love—reading, gardening, whatever fills your cup.
“IVF is as much about your mind as your body. A calm heart can carry you further than you think.” — Ophelia, Fertility Counselor
The IVF Process Step-by-Step for PCOS Patients
Ready to see how IVF unfolds? Here’s a clear, step-by-step look at what happens, with special notes for PCOS.
Step 1: Your First Visit and Tests
It all starts with a fertility specialist. They’ll check:
-
- Hormone levels: Blood tests for FSH, LH, AMH, and more
-
- Ultrasound: To count follicles and check your uterus
-
- Partner’s sperm: If you’re using a partner’s sperm, they’ll test that too
For PCOS, they’ll zoom in on your antral follicle count (AFC)—those little egg sacs. A high AFC (20+) means you might respond strongly to meds.
Step 2: Ovarian Stimulation
You’ll get daily shots to wake up your ovaries and grow multiple eggs. This lasts 8-14 days, with checkups to watch follicle growth.
-
- PCOS Twist: Doctors might use a “low and slow” approach to avoid overstimulating your ovaries and triggering OHSS.
Step 3: The Trigger Shot
When your eggs are ready, a trigger shot (hCG or a GnRH agonist) tells them to mature. For PCOS, the GnRH agonist is often safer—it cuts OHSS risk by 50%, per recent studies.
Step 4: Egg Retrieval
A quick procedure under sedation where a needle grabs the eggs from your ovaries. It takes 20-30 minutes, and you’ll rest afterward.
-
- PCOS Bonus: You might get 15-25 eggs, more than average. But not all may be top-notch.
Step 5: Fertilization
Eggs meet sperm in the lab. It’s either:
-
- Standard IVF: Eggs and sperm mix naturally
-
- ICSI: One sperm is injected into each egg (common if quality’s a worry)
Step 6: Embryo Growth
Embryos grow for 3-5 days. The best ones are picked for transfer.
-
- PCOS Tip: Genetic testing (PGT) can spot healthy embryos if quality’s uneven.
Step 7: Embryo Transfer
A catheter places the embryo in your uterus. It’s fast and painless.
-
- PCOS Option: Freezing embryos and transferring later (FET) can dodge OHSS and give your body a break.
After 10-14 days, a pregnancy test tells you the news.
✔️ Step-by-Step Timeline:
-
- Day 1-14: Stimulation
-
- Day 15: Trigger
-
- Day 17: Retrieval
-
- Day 22: Transfer (or freeze)
-
- Day 32: Test
Success Rates and What Affects Them
So, how likely is IVF to work for you? Let’s look at the numbers and what you can do to tip the scales.
What Studies Say About PCOS and IVF Success
Good news: women with PCOS often have equal or better IVF success rates than others. Why? Those extra follicles mean more eggs and more shots at a healthy embryo. Per the American Society for Reproductive Medicine:
-
- Under 35: 35-45% success per cycle
-
- Over 3 cycles: Up to 70% chance of pregnancy
But it’s not a sure thing. Success hinges on a few factors.
What Influences Your Odds?
-
- Age: Under 35 is the sweet spot; rates drop after 40.
-
- Weight: A BMI over 30 can cut success by 20%. Slimming down helps.
-
- Egg quality: More eggs don’t always mean better eggs. Hormones can play tricks.
-
- Lifestyle: Smoking, stress, and poor diet can drag rates down.
Boosting Your Chances
You’ve got some control here:
-
- Stick to the plan: Take meds on time, hit every appointment.
-
- Eat for fertility: Think Mediterranean—fish, nuts, olive oil.
-
- Try myo-inositol: A 2023 study showed a 15% bump in live births for PCOS patients.
-
- Be patient: One cycle might not do it, but don’t give up.
“Success isn’t just luck—it’s preparation meeting opportunity. PCOS women have a real shot with IVF.” — Caspian Sterling, Reproductive Endocrinologist
Managing Risks and Complications
IVF is safe overall, but PCOS brings a few risks to watch. Knowing them—and how to handle them—keeps you in the driver’s seat.
Ovarian Hyperstimulation Syndrome (OHSS)
OHSS happens when your ovaries go overboard with stimulation. Mild cases (bloating, mild pain) hit 20-30% of PCOS patients; severe ones (breathing trouble, clots) are rare, under 5%.
How to Lower the Risk:
-
- Gentle meds: Lower doses or GnRH antagonists work better for PCOS.
-
- Freeze embryos: Skip the fresh transfer to let your ovaries settle.
-
- Hydrate: Sip electrolyte drinks post-retrieval.
Egg Quality Challenges
PCOS can mean lots of eggs but spotty quality. A 2022 study found 30% of PCOS eggs had chromosomal glitches.
How to Improve:
-
- Metformin: Boosts egg maturity in 25% of cases.
-
- Antioxidants: CoQ10 or vitamin E might help—ask your doc.
-
- Time it right: Pre-IVF lifestyle tweaks can up quality.
Multiple Pregnancies
More eggs can mean twins or more if multiple embryos are transferred. That’s riskier for you and the babies.
How to Avoid:
-
- Single embryo transfer (SET): Just as effective with good embryos, says a 2021 study.
❌ Watch For: Severe OHSS signs—call your doctor if you feel shortness of breath or sharp pain.
Emotional Support: Staying Strong Through IVF
IVF tests more than your body—it tests your spirit. For PCOS patients, the emotional load can feel heavier after years of fertility woes.
What You Might Feel
-
- Hope mixed with fear: Every step brings both.
-
- Exhaustion: The process is long and draining.
-
- Isolation: Friends might not get it.
Ways to Stay Grounded
-
- Connect: Online forums or local groups are goldmines of support.
-
- Therapy: A fertility counselor can be your rock.
-
- Small wins: Celebrate each milestone—egg retrieval, embryo growth.
“You’re tougher than you know. Lean on others, and let yourself feel every part of this.” — Orion Nightingale, Fertility Coach
Cost and Insurance: Planning Your Budget
IVF isn’t cheap, and PCOS can add layers to the bill. Let’s break it down.
How Much Does IVF Cost?
-
- Base cycle: $12,000-$15,000
-
- Meds: $3,000-$5,000
-
- Extras (ICSI, PGT): $1,000-$5,000
PCOS might mean more monitoring or frozen transfers, nudging costs up.
Will Insurance Help?
It depends. Some states mandate IVF coverage; others don’t. PCOS might qualify as a medical need.
-
- Call your insurer: Ask about “infertility due to anovulation.”
-
- Financing: Clinics often have payment plans.
-
- Grants: Check Resolve.org for options.
✔️ Money-Saving Tip: Ask about multi-cycle discounts.
Alternative Therapies: Extra Tools for Success
Beyond IVF, some women with PCOS try add-ons to boost their odds or ease symptoms.
Acupuncture
Needles might sound odd, but a 2023 study found acupuncture upped IVF success by 18% in PCOS patients by boosting ovarian blood flow.
-
- Start: 2-3 months pre-IVF
-
- Frequency: Weekly
Herbal Options
Vitex or cinnamon might balance hormones, but evidence is thin. Check with your doctor—safety first.
Mind-Body Practices
Yoga and meditation cut stress, which a 2022 study linked to better embryo implantation.
-
- Try: Fertility yoga poses like Reclining Bound Angle.
Real Stories: PCOS and IVF Success
Nothing beats hearing from women who’ve been there.
Jamie’s Journey
“PCOS made me feel broken. IVF was scary, but I got 18 eggs, froze them to avoid OHSS, and now my daughter’s 3. It was worth every shot.”
Priya’s Path
“After two failed cycles, I lost hope. Then we adjusted my meds, added myo-inositol, and my son arrived. Don’t give up!”
Conclusion: Your Roadmap to IVF with PCOS
PCOS might complicate your fertility, but IVF opens doors. With smart prep, a solid team, and a little grit, you can navigate this journey. Start with a specialist, tweak your lifestyle, and build your support net—you’ve got this.
Quiz: How Much Do You Know About PCOS and IVF?
Test yourself!
-
- What’s the top fertility issue in PCOS?
-
- A) No sperm
-
- B) No ovulation
-
- C) Blocked tubes
-
- D) No uterus
-
- What’s the top fertility issue in PCOS?
-
- What cuts OHSS risk in PCOS?
-
- A) More eggs
-
- B) GnRH agonist trigger
-
- C) Skipping meds
-
- D) Fresh transfer
-
- What cuts OHSS risk in PCOS?
-
- What boosts IVF success?
-
- A) Weight loss
-
- B) Stress
-
- C) Sugar
-
- D) Smoking
-
- What boosts IVF success?
Answers: 1-B, 2-B, 3-A
Tell Us Your Story
Have you tried IVF with PCOS? Drop your experience below—we’d love to hear it, and it might help someone else!




No comment