Premature Ovarian Insufficiency (POI) – A Comprehensive Guideline
Premature Ovarian Insufficiency (POI), also known as Premature Ovarian Failure or Early Menopause, is a condition that affects many women across the globe. Despite its increasing recognition, there is still a lot of confusion about what POI really is, how it is diagnosed, and how to manage it. In this comprehensive guide, we will explore all the important details about POI, using clear language suited for readers at around an 8th-grade level. Our goal is to help you understand the condition, learn about possible treatments, and discover how to support emotional well-being.
This article combines insights from the top-ranking articles on Google, along with additional in-depth and unique perspectives that are not always fully covered. We will discuss potential causes, risk factors, treatment options, lifestyle tips, recent scientific research, and practical strategies for coping. You will also find advice on fertility, support resources, and how to talk with healthcare providers. By the end, you should feel more informed about POI and empowered to make decisions about your health.
What Is Premature Ovarian Insufficiency (POI)?
Premature Ovarian Insufficiency is a condition in which the ovaries stop functioning properly before a woman turns 40 years old. The ovaries are responsible for producing eggs (ova) and releasing hormones like estrogen and progesterone. When ovarian function stops too soon, it leads to lower levels of these hormones and can cause symptoms similar to those of menopause.
Key Points to Remember
- Age Factor: Normal menopause typically occurs between ages 45-55, but POI happens much earlier (before 40).
- Hormonal Imbalance: POI is linked to lower estrogen levels and irregular or missed periods (amenorrhea).
- Fertility Challenges: POI can make conceiving naturally more difficult, but there are fertility options available.
POI affects about 1 in 100 women under 40 and 1 in 1000 women under 30, according to some estimates. It’s not extremely common, but it’s also not as rare as many people think.
Why Is POI Different from Natural Menopause?
While both POI and menopause involve changes in ovarian function, the biggest difference lies in timing. Natural menopause marks the end of a woman’s reproductive years and usually happens later in life. POI, on the other hand, occurs much earlier and is often unexpected. This can create emotional distress and additional medical concerns because your body experiences hormonal changes before the usual menopausal age.
| Feature | POI (Premature Ovarian Insufficiency) | Natural Menopause |
|---|---|---|
| Typical Age Range | Before age 40 | Between 45-55 |
| Fertility Impact | Sudden, unexpected difficulty conceiving | Gradual decrease in fertility |
| Emotional Response | Often more distressing | More expected, though still varies |
| Hormone Levels | Rapid decline in estrogen | Gradual decline in estrogen |
| Possible Causes | Autoimmune, genetic, iatrogenic, unknown | Natural aging process |
Signs and Symptoms of POI
Many of the symptoms of POI mirror those of menopause, but they usually happen at a younger age. If you suspect you may have POI, watch out for these signs:
-
Irregular or Missed Periods
- Periods may become lighter, less frequent, or stop entirely (amenorrhea).
-
Hot Flashes and Night Sweats
- Sudden feelings of warmth in the upper body, often with sweating or rapid heartbeat.
-
Mood Swings
- Feelings of irritability, sadness, or anxiety without a clear trigger.
-
Vaginal Dryness
- Decreased estrogen can lead to dryness, itching, or discomfort during intercourse.
-
Trouble Sleeping
- Hot flashes and night sweats can disturb restful sleep.
-
Reduced Libido
- Lower hormone levels may affect sexual desire.
-
Fatigue or Low Energy
- Hormonal changes can lead to feelings of tiredness or exhaustion.
-
Difficulty Conceiving
- This might be the first sign that something is off if you’re trying to get pregnant.
Note: If you’re experiencing two or more of these symptoms, it’s a good idea to talk with a healthcare professional. POI is not always the cause, but it is worth investigating.
How Is POI Diagnosed?
Diagnosis often begins with a medical history review and physical exam. Your healthcare provider will look at your symptoms, menstrual cycle patterns, and overall health. If POI is suspected, you may undergo several tests:
-
Blood Tests
- Follicle-Stimulating Hormone (FSH): Elevated FSH levels are a strong indicator of POI.
- Estrogen (Estradiol) Levels: Low estrogen suggests reduced ovarian activity.
- Anti-Müllerian Hormone (AMH): Helps measure ovarian reserve (how many eggs remain).
-
Pelvic Ultrasound
- This imaging test lets doctors see the ovaries and check the number of remaining follicles.
-
Genetic Testing
- Conditions like Fragile X premutation or Turner syndrome can contribute to POI.
-
Autoimmune Screening
- Autoimmune disorders (e.g., thyroid disease) sometimes accompany POI.
-
Bone Density Scan (DEXA)
- Early loss of estrogen can weaken bones, so doctors might check for osteoporosis.
Step-by-Step: POI Diagnosis
- Visit Your Doctor
- Share your symptoms and menstrual history.
- Blood Tests
- Get tested for FSH, estrogen, AMH, and possibly thyroid function.
- Ultrasound
- Check the health of your ovaries.
- Further Genetic or Autoimmune Tests
- If needed, based on initial findings.
- Follow-Up
- Discuss your results and potential treatment plans with your healthcare professional.
Risk Factors and Causes
POI can happen for several reasons, or sometimes for no clear reason at all. Here are some common risk factors and causes:
-
Genetics
- A family history of Fragile X premutation or other genetic conditions can increase your risk.
- Turner Syndrome (when a female has one missing or incomplete X chromosome) can also lead to POI.
-
Autoimmune Disorders
- Diseases like autoimmune thyroid disease, Addison’s disease, and type 1 diabetes sometimes link to early ovarian failure.
-
Medical Treatments
- Chemotherapy or radiation therapy for cancer can damage ovarian tissues.
- Ovarian surgery or procedures that affect ovarian blood supply can also lead to POI.
-
Lifestyle Factors
- Smoking has been shown to speed up ovarian aging.
- Severe stress or poor nutrition might also contribute, though evidence varies.
-
Unknown Causes (Idiopathic)
- Many POI cases remain unexplained.
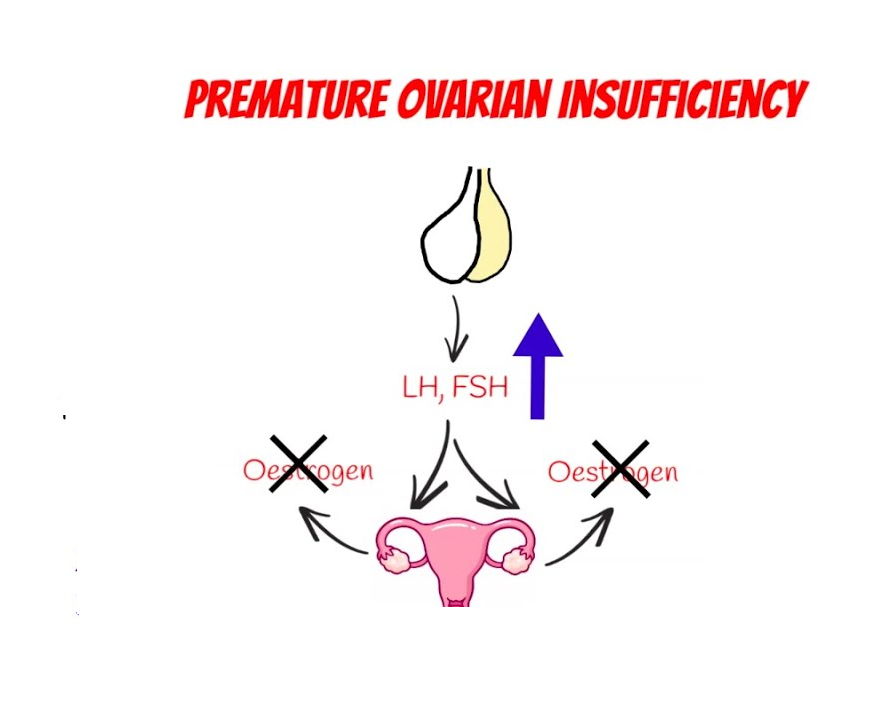
The Role of Hormones in POI
6.1 Estrogen and FSH
Estrogen is the main female hormone responsible for regulating the menstrual cycle, maintaining bone density, and supporting sexual health. Follicle-Stimulating Hormone (FSH) triggers the ovaries to produce mature eggs. In POI:
- Estrogen Levels drop due to reduced ovarian function.
- FSH Levels go up as the body tries to stimulate the ovaries to produce more eggs.
High FSH and low estrogen are strong indicators of POI and help doctors confirm a diagnosis.
6.2 Other Hormones
- Progesterone: Supports the uterine lining and overall menstrual cycle. Usually drops in POI.
- Testosterone: Women produce small amounts of testosterone that help with libido and energy. POI can reduce these levels too.
- Thyroid Hormones: Thyroid disorders can sometimes occur alongside POI.
Treatment Options
If you have POI, treatments often focus on:
- Restoring Hormone Balance
- Supporting Bone Health
- Managing Symptoms
- Addressing Fertility Concerns
Because each woman’s situation is different, treatment plans should be personalized.
1 Hormone Replacement Therapy (HRT)
Hormone Replacement Therapy (HRT) is one of the most common ways to treat POI. It involves taking estrogen (and often progesterone) to help replace the hormones the ovaries are no longer producing.
Benefits of HRT:
- ✔️ Improves menopausal symptoms (hot flashes, night sweats)
- ✔️ Helps maintain bone density and reduce the risk of osteoporosis
- ✔️ Can improve sexual health by reducing vaginal dryness
- ✔️ Often stabilizes mood and may improve energy levels
Potential Risks/Considerations:
- ❌ Slight increase in the risk of blood clots (especially if you have certain genetic factors)
- ❌ May not be suitable for women with specific health issues like certain cancers
Most doctors consider HRT for women with POI until the typical age of menopause (around age 50) to protect long-term bone and heart health, unless there are specific reasons not to use it.
2 Non-Hormonal Treatment Options
For women who cannot or choose not to use HRT, there are other options:
-
Selective Serotonin Reuptake Inhibitors (SSRIs)
- Medications like paroxetine can help manage hot flashes and mood swings.
-
Herbal Supplements
- Some women use black cohosh, red clover, or phytoestrogens (plant-based estrogens).
- Scientific evidence varies, so talk with your doctor before starting any supplement.
-
Bone Density Management
- Calcium and Vitamin D supplements can help maintain bone health.
- Bisphosphonates (e.g., alendronate) are sometimes considered if bone density is already compromised.
-
Lifestyle Changes
- Low-impact exercise, stress management, and a balanced diet can ease some symptoms and support overall well-being.
3 New and Emerging Therapies
Researchers are continually looking for new ways to manage or even reverse some effects of POI. While not yet standard practice, some emerging areas include:
-
Platelet-Rich Plasma (PRP) Therapy
- PRP injections into the ovaries have shown early promise in improving ovarian function in some small studies.
- Still considered experimental with limited long-term data.
-
Stem Cell Therapy
- Research is underway on whether stem cells can stimulate new follicle growth in damaged ovaries.
- More human trials are needed to confirm safety and effectiveness.
-
Gene Therapies
- Very early research aims to correct certain genetic causes of POI, but this is not yet available as a standard treatment.
Remember: Always consult a qualified medical professional before trying any experimental therapies.
Lifestyle Changes for Better Ovarian Health
Lifestyle has a significant impact on hormonal balance. While you can’t control your genes or certain medical causes, you can influence everyday habits to support overall health.
8.1 Balanced Diet
- Focus on Nutrient-Dense Foods: Fruits, vegetables, whole grains, lean proteins, and healthy fats.
- Calcium and Vitamin D: Crucial for bone health. Include dairy or fortified products, leafy greens, and maybe a supplement if levels are low.
- Avoid Excess Sugar and Processed Foods: These can contribute to energy crashes and weight gain.
8.2 Regular Exercise
- Weight-Bearing Workouts: Walking, hiking, or light jogging help maintain bone density.
- Strength Training: Increases muscle mass and supports healthy bones.
- Yoga and Pilates: Improve flexibility and reduce stress.
8.3 Stress Management
- Mindfulness and Meditation: Can reduce anxiety and stabilize mood swings.
- Adequate Sleep: Aim for 7-9 hours per night to help regulate hormones.
- Relaxation Techniques: Deep breathing, gentle stretching, or warm baths.
8.4 Avoid Smoking and Limit Alcohol
- Smoking can hasten ovarian aging.
- Excessive Alcohol can worsen symptoms like hot flashes and disrupt sleep.
Emotional and Mental Well-Being
Receiving a POI diagnosis can be overwhelming. It might bring feelings of grief, anger, confusion, or fear—especially if you have been hoping to start or expand your family.
Common Emotional Challenges
- Sudden Change of Life Plans: Fertility may be affected earlier than expected.
- Body Image Concerns: Physical changes, weight gain, or mood swings can affect self-esteem.
- Relationship Strain: POI can impact intimacy and communication with partners or family members.
How to Cope
- Therapy or Counseling
- Talking to a professional can help process emotions and develop coping strategies.
- Support Groups
- Online forums and local groups let you connect with others experiencing the same challenges.
- Open Communication
- Share how you feel with close friends or family to receive emotional support.
- Mindful Practices
- Journaling or guided meditation can ease stress and improve clarity.
Remember: Emotional wellness is just as important as physical wellness. If you feel overwhelmed, don’t hesitate to seek professional help.
Fertility and Family-Building Options
One of the most distressing aspects of POI can be the worry about having children. While fertility is reduced, there are still possible options.
10.1 Fertility Treatments
- In Vitro Fertilization (IVF): If you still produce viable eggs, IVF may increase your chances of conception.
- Egg Donation: Donor eggs can be fertilized with your partner’s sperm (or donor sperm) and then placed into your uterus.
- Surrogacy: Another woman carries the pregnancy to term using your eggs (if possible) or donor eggs.
10.2 Natural Pregnancy After POI
Although spontaneous ovulation can still occur in some women with POI, it is less likely. This can sometimes lead to a spontaneous pregnancy. However, it is unpredictable and should be discussed with a reproductive endocrinologist for realistic expectations.
10.3 Adoption and Foster Care
If medical options are not desirable or feasible, many women and couples choose:
- Adoption
- Fostering a Child
These paths provide the chance to form a loving family without relying on fertility treatments.
Myths vs. Facts About POI
Myth 1: POI means you’ll never get pregnant.
- Fact: While fertility is lower, some women do conceive naturally, and fertility treatments can help many others.
Myth 2: Only older women get POI.
- Fact: By definition, POI occurs before age 40, and in rare cases, even in the teens or early twenties.
Myth 3: HRT always causes cancer.
- Fact: HRT has risks and benefits, but for younger women with POI, the benefits often outweigh the risks until the normal age of menopause.
Myth 4: POI is completely curable.
- Fact: There is no guaranteed cure. However, symptoms can be managed, and new research may lead to breakthroughs in the future.
Myth 5: You did something wrong to cause POI.
- Fact: Most cases of POI are beyond your control, involving genetics, medical treatments, or unknown factors.
Frequently Asked Questions (FAQs)
Q1: Can stress alone cause POI?
A1: Chronic stress can affect hormone levels, but it rarely directly causes POI. It can contribute to irregular periods, but POI usually has a more complex origin.
Q2: How often should I see a doctor if I have POI?
A2: It’s recommended to have regular check-ups every 6-12 months to monitor hormone levels, bone density, and general health.
Q3: Does POI increase the risk of other health problems?
A3: Yes, lower estrogen can affect bone density, heart health, and sexual health. Working closely with your doctor can help reduce these risks.
Q4: Will I still have menstrual periods on HRT?
A4: You might experience some withdrawal bleeding or a “fake” period when on combined hormone therapy, but it doesn’t necessarily mean normal ovulation has returned.
Q5: Are there any natural remedies for hot flashes?
A5: Lifestyle strategies like layering clothing, staying hydrated, and using cooling fans can help. Some herbal supplements (like black cohosh) may offer mild relief, but talk with a healthcare provider first.
Practical Tips and Step-by-Step Guide
Below is a step-by-step outline to guide you from diagnosis through management:
-
Confirm the Diagnosis
- Schedule a medical appointment if you have irregular periods or suspect POI.
- Request FSH, estrogen, and AMH tests.
- Undergo an ultrasound if recommended.
-
Discuss Treatment Options
- Ask about Hormone Replacement Therapy (HRT).
- Consider non-hormonal treatments if HRT isn’t suitable for you.
- Talk about supplements for bone health (e.g., calcium, vitamin D).
-
Fertility Counseling
- Consult a reproductive endocrinologist to explore IVF, donor eggs, or other assisted reproductive technologies.
- Discuss natural pregnancy chances and plan accordingly.
- Look into adoption or foster care if desired.
-
Address Emotional Needs
- Seek counseling if feeling stressed or depressed.
- Join support groups or online forums for shared experiences.
- Practice mindfulness and stress reduction techniques.
-
Lifestyle Management
- Exercise regularly (weight-bearing activities, yoga, or swimming).
- Adopt a balanced diet rich in nutrients.
- Avoid or reduce smoking and excess alcohol.
-
Regular Check-Ups
- Monitor bone density via DEXA scans.
- Keep track of hormone levels periodically.
- Update your healthcare provider about any new symptoms.
-
Stay Informed
- Keep up with the latest research on new therapies like PRP or stem cells.
- Attend educational seminars or read reliable medical sources for updates.
- Advocate for yourself: Ask questions and seek second opinions when needed.
Key Takeaways
-
POI Can Happen to Anyone
- It is not limited to older women or women with certain lifestyles.
-
Early Diagnosis Is Crucial
- The sooner you address hormone imbalances, the better your long-term health outlook.
-
Treatment Is Tailored
- Options like HRT, alternative therapies, and lifestyle changes are unique to each individual.
-
Fertility Help Exists
- IVF, donor eggs, and adoption can help you start or grow a family if POI impacts your fertility.
-
Emotional Support Matters
- Counseling, support groups, and open discussions with loved ones can provide vital emotional relief.
-
Ongoing Research
- Innovative treatments like PRP and stem cell therapy are emerging, but more studies are needed.
Interactive Conclusion
Premature Ovarian Insufficiency can feel like an unexpected detour in your life journey. However, understanding the condition and exploring the right treatment options can help you regain control and live a healthy, fulfilling life. Remember: you’re not alone, and resources are available to guide you every step of the way.
We’d Love to Hear From You
- Have you or someone you know experienced POI?
- What was the biggest challenge, and how did you overcome it?
Share your thoughts or personal tips in the comments section below. By talking openly about POI, we can all learn from each other’s experiences and offer support to those just beginning their journey.
Disclaimer: This article is for informational purposes only and does not substitute medical advice. Always consult a qualified healthcare professional for personalized diagnosis and treatment options.

No comment