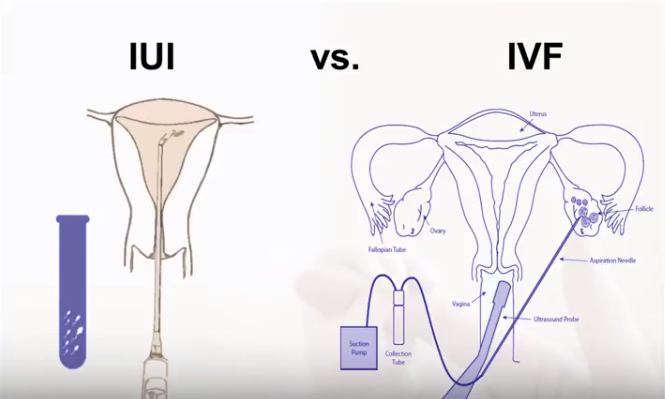
If you’ve been trying to start or grow your family, chances are you’ve come across the terms IUI and IVF. These two fertility treatments are often mentioned in the same breath, yet they differ in significant ways. How do you know which option is right for you? What’s the difference between IUI vs. IVF in terms of costs, success rates, and time commitment? And how can you prepare for the emotional journey that often comes with fertility treatments?
In this in-depth blog post, we’ll explore these questions and more. We’ll walk you through the key facts, highlight the latest research, offer easy-to-follow checklists, and provide tips for your next steps. By the end, you’ll have a clearer understanding of what IUI and IVF entail, allowing you to make the best decision for you and your family.
What Is IUI?
IUI stands for Intrauterine Insemination. It’s sometimes referred to as “artificial insemination.” Think of IUI as a simpler, more direct way to get sperm closer to the egg.
The Basic Process of IUI
-
Sperm Collection and Preparation:
- A semen sample is collected (usually from a partner or donor).
- The lab processes (“washes”) the sperm to remove any debris or slower-moving sperm cells, so that only the healthiest, most motile sperm remain.
-
Timing of Ovulation:
- The patient may track ovulation through at-home kits or via fertility medication prescribed by a healthcare provider.
- The goal is to pinpoint the fertile window—the few days each cycle when fertilization is most likely.
-
Insertion of Sperm:
- A thin catheter is used to place the sperm directly into the uterus.
- This procedure is quick, usually painless, and often takes just a few minutes.
-
Waiting Game:
- After insemination, you wait around two weeks to take a pregnancy test. This period is commonly known as the “two-week wait” (2WW).
Why People Choose IUI
- Less Invasive: Compared to IVF, IUI involves fewer medical procedures.
- Lower Cost: IUI cycles are typically cheaper than IVF cycles.
- Good Starting Point: Many couples or individuals with mild fertility issues try IUI before moving on to more complex treatments like IVF.
Ideal Candidates for IUI
- Mild Male Factor Infertility: When sperm count or motility is only slightly below normal.
- Unexplained Infertility: When tests don’t identify a clear cause.
- Cervical Factors: Situations where cervical mucus might hinder sperm from reaching the egg.
- Same-Sex Couples or Single Parents: IUI is often used with donor sperm to achieve pregnancy.
Key Point: If blocked fallopian tubes or severe male infertility are present, IUI may not be effective. Always consult a fertility specialist to determine eligibility.
Potential Downsides of IUI
- Lower Success Rate (compared to IVF): Often around 10-20% per cycle, though rates vary based on age and fertility diagnoses.
- Possible Use of Medication: Some people need ovulation-stimulating drugs, which can lead to multiple pregnancies or mild side effects.
- Multiple Cycles: You may need to repeat IUI several times before achieving pregnancy or moving on to IVF.
What Is IVF?
IVF stands for In Vitro Fertilization. Literally translated, “in vitro” means “in glass,” referencing the lab dish where fertilization occurs. IVF is more complex than IUI and involves multiple stages.
The Basic Process of IVF
-
Ovarian Stimulation:
- The patient takes fertility medications (injections or pills) to stimulate the ovaries to produce multiple follicles (each containing an egg).
- Frequent ultrasounds and blood tests check how the follicles are growing.
-
Egg Retrieval:
- A minor surgical procedure, often under mild sedation.
- A healthcare provider uses a thin needle to collect eggs from the ovaries.
-
Fertilization in the Lab:
- Sperm (from a partner or donor) is introduced to the eggs in a lab dish.
- In ICSI (Intracytoplasmic Sperm Injection), a single sperm is injected directly into each egg, which helps if there are male factor issues.
-
Embryo Culture and Development:
- Fertilized eggs (embryos) are monitored in a specialized incubator for several days (3-5 days, sometimes longer).
-
Embryo Transfer:
- A selected embryo (or embryos) is placed into the uterus with a thin catheter. This step is usually painless, similar to IUI.
- Any additional viable embryos may be frozen for future use (known as embryo cryopreservation).
-
Two-Week Wait:
- Similar to IUI, you wait around two weeks before taking a pregnancy test to find out if the cycle was successful.
Why People Choose IVF
- Higher Success Rates: Especially for those under 35 or with healthy ovarian reserve. Success rates can be around 40-50% or more per cycle in some cases, though it varies by clinic and personal factors.
- Addresses Multiple Fertility Problems: Helps when there are issues like blocked tubes, advanced maternal age, or severe male factor infertility.
- Opportunity for Genetic Testing: PGT-A (Preimplantation Genetic Testing for Aneuploidies) checks embryos for chromosomal abnormalities before transfer, potentially increasing the odds of a healthy pregnancy.
- Embryo Freezing: Extra embryos can be frozen for later use, offering future cycles without the need for another full ovarian stimulation.
Potential Downsides of IVF
- Higher Cost: IVF cycles can be quite expensive, ranging from several thousand to tens of thousands of dollars, depending on your region and insurance coverage.
- More Invasive: Requires injections, egg retrieval, and frequent monitoring.
- Emotional Stress: The complexity of IVF can be emotionally taxing.
Tip: If finances are a concern, some clinics offer shared-risk or bundle packages. Research local resources or speak to a financial counselor at your fertility clinic.
IUI vs. IVF: Key Differences at a Glance
Below is a comparison table that highlights the main contrasts:
| Factor | IUI | IVF |
|---|---|---|
| Procedure Complexity | Simple, non-surgical sperm insertion | Involves egg retrieval, fertilization in lab, embryo transfer |
| Average Cost | Lower cost (often $300 – $2,000 per cycle, depending on medication and location) | Higher cost (can range from $10,000 – $20,000+ per cycle, plus medication costs) |
| Success Rates | ~10–20% per cycle (varies by age, fertility factors) | ~40–50%+ for women under 35; decreases with age |
| Time Commitment | Minimal (a few clinic visits, timing insemination) | Intensive (monitoring appointments, egg retrieval, lab work, etc.) |
| Ideal Candidates | Mild male factor infertility, unexplained infertility, or cervical issues; also for single parents, same-sex couples | Serious male factor infertility, blocked tubes, advanced maternal age, or repeated failed IUI; can also use PGT-A |
| Medication Use | Optional or lower doses (some IUI cycles are “natural” or use minimal medication) | Typically higher doses of fertility medication to stimulate multiple eggs |
| Risks | Mild risk of multiple pregnancy when using fertility drugs | Ovarian Hyperstimulation Syndrome (OHSS), multiple pregnancies, emotional stress |
(Cost estimates and success rates can vary based on region, clinic, and individual medical profiles.)
Success Rates—What the Numbers Really Mean
Breaking Down IUI Success Rates
- Age Matters: Women under 35 generally see higher success rates (15-20% per IUI cycle), while women over 40 often experience lower rates (5-10% or less per cycle).
- Health Factors: Uterine health, sperm quality, and lifestyle (smoking, weight issues) can significantly impact outcomes.
- Medication vs. Natural Cycle: If you use fertility medication to stimulate ovulation, you might increase your chances of a successful IUI, but you also raise the risk of twins or triplets.
Breaking Down IVF Success Rates
- Clinic Variations: Different fertility clinics report varying success rates, so it’s wise to check your clinic’s statistics through reputable databases (like SART in the U.S.).
- Embryo Quality: The better the embryo quality, the higher the chance of implantation.
- PGT-A Testing: Screening embryos for chromosomal abnormalities can boost success rates, particularly for older patients or those with recurrent miscarriage.
- Cumulative Success: If you have multiple good embryos, your chance of eventually having a baby over several embryo transfers often exceeds 60-70% (for younger patients).
Reading Between the Lines
- Per-Cycle vs. Per-Pregnancy: A “success rate” often means a live birth per cycle attempt, not just a positive pregnancy test.
- Cumulative Rates: While one IVF cycle might have a success rate of 40%, three consecutive cycles might push overall success to 70% or more.
- Context Matters: Both IUI and IVF success depend on personal circumstances, such as age, lifestyle, and specific fertility challenges.
Remember: These figures are averages and can’t predict individual outcomes. Consult with a reproductive endocrinologist for a more tailored prognosis.
Cost Comparisons: IUI vs. IVF
Typical Financial Outlays
-
IUI:
- Basic Cycle: Sperm preparation, insemination, lab fees.
- Medication Costs: Extra if fertility drugs are used.
- Range: Usually $300 – $2,000 per cycle, but can be higher in major cities or private clinics.
-
IVF:
- Cycle Fee: Covers monitoring, egg retrieval, embryo culture, and embryo transfer.
- Medication Costs: Fertility drugs can run thousands of dollars.
- Additional Options: PGT-A testing, ICSI, and embryo freezing come with extra fees.
- Range: Often $10,000 – $20,000+ per cycle.
Insurance and Financing
- Check Your Coverage: Some states or countries require insurance companies to cover certain fertility treatments.
- Payment Plans or Discounts: Many clinics offer financing options. Some also have discount programs for military families, teachers, or first responders.
- Shared-Risk Programs: You pay a set fee for multiple IVF cycles, often with a portion refunded if you don’t achieve a successful pregnancy.
The Risk of “Doing Many IUIs”
Because IUI is less expensive per cycle, some couples try many IUI cycles before switching to IVF. But multiple IUI attempts can add up in cost. If the probability of success with IUI is low, you might consider moving to IVF sooner to save both time and emotional energy.
Factors That May Influence Your Choice
1. Medical Diagnosis
- Blocked or Removed Fallopian Tubes: IVF is generally the only viable option.
- Severe Male Factor Infertility: IVF with ICSI is often recommended.
- Mild Male Factor / Cervical Issues: IUI could be enough.
2. Age and Ovarian Reserve
- Under 35: May opt for IUI first, if other conditions are favorable.
- Over 35 or Low Ovarian Reserve: IVF could offer higher success in a shorter timeframe.
3. Emotional and Mental Health
- Stress Tolerance: IVF involves more intense procedures and emotional stress, but multiple IUI failures can be equally draining.
- Support System: Consider if you have emotional support from partners, friends, or counseling services.
4. Time Constraints
- Younger Women: Might have time to try IUI for a few cycles.
- Older Women: Often shift to IVF faster due to declining fertility rates with age.
5. Personal Preference
Some people prefer starting with the least invasive treatment, even if it means multiple attempts. Others want the highest possible success rate right away and opt for IVF.
Potential Risks and Side Effects
IUI Risks
- Mild Discomfort: Spotting or cramping after insemination.
- Infection: Rare but possible if bacteria enter the uterus during the procedure.
- Multiple Pregnancy: More likely if ovulation-inducing medication is used.
IVF Risks
- Ovarian Hyperstimulation Syndrome (OHSS): This can occur if the ovaries are overstimulated by fertility meds, leading to swelling and fluid buildup.
- Multiple Pregnancy: IVF transfers more than one embryo sometimes, increasing the risk of twins or triplets (though many clinics now encourage single-embryo transfers).
- Emotional Strain: The ups and downs of IVF can be tough, and support systems are crucial.
- Surgical Risks: Egg retrieval is minimally invasive, but any procedure with sedation has potential risks like bleeding or infection.
Monitoring and Minimizing Risks
- Frequent Check-Ups: Ultrasounds and blood tests help doctors catch early signs of OHSS or other issues.
- Single-Embryo Transfer: Lowers the chance of multiple pregnancy while maintaining strong success rates for those with healthy embryos.
- Counseling: Mental health support is key to navigating the emotional roller coaster of fertility treatment.
Step-by-Step Look at an IUI Cycle
To give you a clearer idea, here’s a simplified breakdown of how an IUI cycle might unfold:
- Day 1: First day of menstrual cycle.
- Medication or Natural Cycle?: You might start fertility medication (like Clomid or letrozole) or proceed naturally.
- Monitoring: Ultrasounds to check follicle development.
- Ovulation Trigger: If using medication, you might get a “trigger shot” (hCG injection) to time ovulation.
- IUI Procedure: Around 24-36 hours after the trigger shot, the washed sperm is inserted into the uterus.
- Two-Week Wait: Avoid overthinking (easier said than done!), and then test for pregnancy.
Possible Next Steps: If unsuccessful, consult with your doctor about whether to try another cycle or move to IVF.
Step-by-Step Look at an IVF Cycle
An IVF cycle is more involved. Here’s a general outline:
-
Ovarian Stimulation (1-2 Weeks)
- You self-administer fertility injections.
- Regular ultrasound and blood tests track follicle growth.
-
Trigger Shot
- Once follicles reach the right size, you’ll take an hCG (or similar hormone) injection to mature the eggs.
-
Egg Retrieval (Typically Day 12-14)
- Done under light anesthesia or sedation.
- The doctor collects the eggs using an ultrasound-guided needle.
-
Fertilization in the Lab
- Eggs and sperm are combined in a dish (or via ICSI).
- The resulting embryos are monitored for development.
-
Embryo Transfer (Day 3 or Day 5)
- A healthy embryo (or embryos) is transferred into the uterus.
- Remaining embryos may be frozen for future use.
-
Luteal Phase Support
- You might take progesterone supplements to help support implantation.
-
Pregnancy Test (~2 Weeks Later)
- You’ll visit the clinic or use a blood test to confirm pregnancy.
Emotional Well-Being and Coping Strategies
IUI Emotional Landscape
- Hope vs. Disappointment: Each month can feel like a fresh start, but repeated IUI failures can accumulate emotional stress.
- Lower Pressure?: Some people find IUI less emotionally taxing than IVF due to fewer medications and shorter procedures.
IVF Emotional Landscape
- High Stakes: The financial and physical effort invested in IVF can make failures more devastating.
- Support System: Online forums, in-person support groups, or therapy sessions can offer a safe place to share feelings.
- Mind-Body Techniques: Activities like yoga, meditation, or journaling can help reduce stress.
Helpful Coping Tips
- Set Realistic Expectations: Understand that success might not happen on the first try.
- Communicate Openly: Talk to partners, friends, or counselors about how you feel.
- Self-Care Routines: A warm bath, a walk in nature, or a creative hobby can boost mood during waiting periods.
- Join a Support Group: Connecting with others who share similar experiences can offer comfort and advice.
Common Myths About IUI and IVF
Myth 1: “IVF Always Results in Twins or Triplets”
- Reality: Single-embryo transfer has become more common, drastically reducing multiple pregnancies. Many IVF clinics focus on healthy singleton pregnancies.
Myth 2: “IUI Is Always Successful on the First Try”
- Reality: Some couples succeed on their first IUI cycle, but many require multiple attempts. Others may need IVF if IUI fails repeatedly.
Myth 3: “Only Older Women Use IVF”
- Reality: Women in their 20s and 30s also use IVF for various reasons (blocked tubes, endometriosis, low sperm count in partner, etc.).
Myth 4: “Stress Makes Treatment Useless”
- Reality: While stress isn’t helpful, there’s no solid proof that stress alone will cancel out the possibility of getting pregnant. Emotional well-being is important but doesn’t guarantee outcomes.
Latest Research and Innovations
Personalized Medicine in Fertility
- Genetic Testing: Beyond PGT-A, there are tests to check for genetic diseases (PGT-M). This helps transfer only embryos free from specific conditions.
- ReceptivaDx: A test that looks for markers of endometriosis or uterine inflammation that could hinder implantation.
Advancements in Lab Techniques
- Time-Lapse Embryo Monitoring: Specialized incubators allow embryologists to watch embryo development in real-time without exposing them to external conditions.
- Artificial Intelligence: Some clinics use AI to help select the best embryo, analyzing minute details invisible to the human eye.
Cryopreservation Improvements
- Vitrification: A fast-freezing method that has increased embryo survival rates. This means more people opt for elective embryo freezing or preserve fertility by freezing eggs earlier in life.
Natural Cycle IVF
- Lower Medication Use: Some clinics offer “mini-IVF” or “natural cycle IVF,” where fewer fertility drugs are used. This can be an alternative for women who respond poorly to high-dose stimulation or prefer a less intense approach.
Practical Tips and Checklists
Checklist: Preparing for Your Doctor’s Visit
- ✔️ Gather Medical Records: Any previous fertility tests, medical history, surgeries, etc.
- ✔️ List Your Questions: Don’t rely on memory; note down your concerns and curiosities.
- ✔️ Budget Research: Have a rough idea of your financial limits or insurance coverage.
- ✔️ Emotional Readiness: Talk to your partner or a friend about how you’re feeling ahead of the appointment.
Checklist: Lifestyle Considerations for Fertility
| Lifestyle Factor | Recommendation |
|---|---|
| Diet | Focus on whole foods, lean proteins, fruits, veggies; consider prenatal vitamins. |
| Exercise | Moderate activity is beneficial (e.g., brisk walking, yoga). Avoid overly intense workouts during treatment. |
| Caffeine | Limit intake (1–2 cups of coffee or less). |
| Alcohol | Many doctors suggest minimal or zero alcohol when trying to conceive. |
| Smoking | Strongly advised to quit (for both partners) as it affects egg and sperm quality. |
| Stress | Incorporate relaxation techniques: meditation, journaling, or counseling. |
Checklist: Questions to Ask Your Fertility Specialist
- **Which treatment do you recommend for my situation—IUI or IVF—and why?
- What is the estimated cost of this treatment, including medication, lab work, and any extras (like PGT-A)?
- How many cycles of IUI do you usually advise before considering IVF?
- What are the main risks for me, and how can we minimize them?
- Success rates at your clinic for someone of my age and diagnosis?
- Support services available, like counseling or support groups?
Real-Life Stories
Emily and Jake: IUI Success After a Few Tries
- Background: Emily (age 32) and Jake (age 34) had been trying to conceive for over a year. Tests showed mild male factor infertility and slightly irregular cycles.
- Treatment: Their doctor suggested starting with IUI. They tried two cycles with oral fertility medication.
- Outcome: On the third IUI cycle, Emily became pregnant. She gave birth to a healthy baby boy. The total cost was lower than a single IVF cycle, making IUI a good choice for them.
Sarah and Linda: Moving Quickly to IVF
- Background: Sarah (38) and Linda (36) wanted to use donor sperm to start their family. At Sarah’s age, her doctor recommended maximizing their chances quickly.
- Decision: After one failed IUI, they chose IVF with a single-embryo transfer.
- Outcome: Sarah conceived on their first IVF attempt. Though IVF was costly, they felt it was worth the higher success rate, considering Sarah’s age.
James and Alex: Severe Male Factor Infertility
- Background: James and Alex needed a surrogate and donor eggs to start a family, as James had a very low sperm count.
- Treatment: IVF with ICSI was the clear choice. They found an egg donor, used James’s sperm, and transferred the best embryo into their chosen surrogate.
- Outcome: While it took two IVF cycles to achieve a pregnancy, they now have a beautiful daughter. IUI was never a viable option due to the severity of male factor issues.
Deciding Between IUI and IVF: A Deeper Look
When IUI Might Be Your First Choice
- You’re younger (under 35) with mild or unexplained fertility issues.
- You prefer a less invasive procedure to start with and don’t mind trying multiple cycles.
- Your finances or insurance coverage favor lower-cost treatments first.
When IVF Might Be Your First (or Next) Choice
- You have significant male factor infertility, blocked fallopian tubes, or advanced maternal age.
- You’ve tried multiple IUIs with no success and want a higher success rate.
- You’re considering genetic testing or have a history of miscarriages.
Trust Your Gut—and Your Doctor
While statistics and costs are important, fertility decisions also hinge on your instincts, mental health, and personal circumstances. A skilled reproductive endocrinologist can provide data-driven guidance, but ultimately the choice is yours.
Additional Resources and Reading
-
SART (Society for Assisted Reproductive Technology):
- https://www.sart.org/
- Offers clinic success rate comparisons in the U.S.
-
ASRM (American Society for Reproductive Medicine):
- https://www.asrm.org/
- Features guidelines, fact sheets, and news on fertility treatments.
-
Resolve: The National Infertility Association:
- https://resolve.org/
- Provides support, local groups, and advocacy resources.
Common FAQs About IUI vs. IVF
Q1. Is IUI less painful than IVF?
A: Generally, yes. IUI is usually quick and pain-free, similar to a pap smear. IVF requires injections, blood draws, and an egg retrieval procedure, which can involve mild discomfort or sedation.
Q2. Can I do IUI without fertility medications?
A: Yes, a “natural cycle IUI” is possible. However, using medication can boost the chances of a successful pregnancy by encouraging the growth of multiple follicles.
Q3. How many IUI attempts should I try before moving on to IVF?
A: It depends on factors like age, health, and financial considerations. Some doctors suggest 3-4 IUI attempts before discussing IVF, but this can vary.
Q4. Does IVF guarantee a baby?
A: No. While IVF offers higher success rates, there is no guarantee. Age, genetics, and overall health play major roles in determining outcomes.
Q5. Is it risky to have twins or triplets with IUI or IVF?
A: Using fertility drugs in IUI can lead to multiple eggs, raising the possibility of twins or more. In IVF, transferring multiple embryos can lead to multiples, but many clinics recommend single-embryo transfer to reduce the risk.
Final Thoughts on the IUI vs. IVF Decision
Choosing between IUI and IVF can feel overwhelming, but remember—you don’t have to figure it all out alone. Fertility specialists, counselors, and support groups are there to help you understand your options. Ultimately, the goal is to increase your chances of having a healthy pregnancy in a way that fits your medical situation, timeline, and emotional comfort.
IUI might be the first step for some, especially if you’re dealing with mild fertility challenges and want a less expensive, less invasive option. However, IVF typically offers higher success rates and is more versatile in addressing complicated diagnoses, such as advanced age or severe male factor infertility.
Weigh your financial resources, time constraints, emotional well-being, and doctor’s advice. Most importantly, give yourself the compassion, patience, and support you need along the way. Fertility journeys can be emotional roller coasters—but they can also be transformative experiences that bring you closer to your dream of parenthood.
We want to hear from you:
- What worries you the most about IUI or IVF?
- Which factor (cost, time, success rates, or emotional toll) influences your decision the most?
- Have you tried any coping strategies or support groups that made a difference?
Share your experiences or questions in the comments below—or reach out on social media. Your story might just help someone else feel less alone on this path!




No comment