
Ovarian cysts are common fluid-filled sacs that form on or inside a woman’s ovaries. You may have heard about them and wondered: Are they dangerous? Can they affect my chances of getting pregnant? The short answer is: It depends on the type of cyst and your overall health. In many cases, ovarian cysts are harmless and resolve on their own. Other times, they can create complications, including possible effects on fertility.
In this article, we’ll take a deep dive into ovarian cysts and their relationship to fertility. We’ll discuss what they are, why they happen, the different types, and which ones are more likely to affect your ability to conceive. We’ll also go over ways to detect, manage, and even prevent them whenever possible. If you’ve been searching for a thorough, easy-to-understand guide on ovarian cysts and infertility, you’ve come to the right place.
What Exactly Are Ovarian Cysts?
An ovarian cyst is a fluid-filled sac that grows in or on the surface of an ovary. The majority of ovarian cysts are benign (noncancerous), and many women may not even notice they have one because these cysts often come and go without causing any symptoms. The most common type of ovarian cyst forms as part of the normal menstrual cycle and goes away on its own within a few weeks or months.
However, some cysts can grow larger, last longer, or cause health problems such as pain, hormonal imbalances, or in rare cases, ovarian damage. When this happens, women might worry if these cysts could lead to issues with getting pregnant or carrying a pregnancy. Understanding the types of cysts is an important first step in figuring out whether they pose a threat to fertility.
Types of Ovarian Cysts
Not all ovarian cysts are alike. Some occur naturally (functional cysts) as part of ovulation, while others may arise from hormonal disorders, endometriosis, or other conditions. Below is a simplified overview:
| Type of Ovarian Cyst | Description | Effect on Fertility |
|---|---|---|
| Functional Cysts | Form during the normal menstrual cycle (follicular cysts and corpus luteum cysts). They usually go away on their own. | Often do not cause infertility unless they grow large or are associated with other problems. |
| Polycystic Ovaries (PCOS) | Multiple small cysts on the ovaries due to hormonal imbalance (part of Polycystic Ovary Syndrome). | Can disrupt ovulation, making conception harder. |
| Endometriomas | Occur when endometrial tissue (the lining of the uterus) grows on the ovaries (linked to endometriosis). | May affect egg quality and interfere with ovarian function. |
| Dermoid Cysts | Contain various types of tissues (hair, fat, bone). They typically grow slowly and can become large. | Less common cause of fertility issues but can sometimes lead to complications if not treated. |
| Cystadenomas | Develop from cells on the outer surface of the ovary; can be filled with a watery or mucous material. | Might cause ovarian twisting or rupture if large, but not always directly linked to infertility. |
| Hemorrhagic Cysts | Functional cysts that bleed internally. Can cause pain and discomfort. | Usually do not directly affect fertility but can cause complications if large or ruptured. |
Functional Cysts
Functional cysts happen when your ovary goes through its normal monthly cycle. Each month, an egg grows inside a tiny sac called a follicle. Sometimes, the follicle doesn’t release the egg or doesn’t shrink after releasing the egg. This can lead to a fluid-filled pocket known as a follicular cyst. There is also a type of functional cyst called a corpus luteum cyst, which occurs after the egg is released. These cysts usually go away on their own and typically don’t cause long-term fertility issues.
Polycystic Ovary Syndrome (PCOS)
PCOS is a hormonal disorder that can lead to multiple small cysts on the ovaries. It’s a common cause of infertility because it disrupts normal ovulation. Women with PCOS often experience irregular periods, elevated levels of androgens (male hormones), weight gain, and other symptoms.
- Core point: PCOS is a leading endocrine disorder that can result in fertility challenges.
- Scientific support: According to research published in the Journal of Clinical Endocrinology & Metabolism, PCOS is a major cause of anovulation (lack of ovulation), which directly impacts fertility.
- Practical tip: If you suspect PCOS due to irregular periods or other symptoms, see a healthcare provider for hormonal testing and an ultrasound.
Endometriomas
Endometriomas occur when tissue similar to the lining of the uterus (endometrium) grows on or in the ovaries. These are often called “chocolate cysts” due to the dark brown fluid inside them. Endometriomas can harm fertility by affecting the health of the ovaries and eggs. Women with endometriomas may also have endometriosis in other parts of the reproductive system, leading to painful periods and possible scarring around the pelvic organs.
Dermoid Cysts
Dermoid cysts can contain a variety of tissues such as hair, teeth, or bone. They typically grow slowly and might not produce symptoms until they become large. Though they’re not commonly linked to infertility, very large dermoid cysts may cause ovary twisting (ovarian torsion) or damage that can affect fertility.
Cystadenomas
Cystadenomas come from cells on the outer lining of the ovary and can fill with fluid or mucus. They can grow quite large and sometimes cause pain or bloating. While they are often benign, large cystadenomas can increase the risk of ovarian torsion and affect ovarian blood flow, potentially interfering with fertility if not managed.
Ovarian Cysts and Infertility: The Connection
One of the most frequent questions women have is, “Do ovarian cysts cause infertility?” The answer depends on various factors, such as the type of cyst, its size, and how it affects ovulation. Let’s break down the main ways ovarian cysts can impact fertility:
-
Ovulation Interference
- Certain cysts, particularly those associated with PCOS, can keep an egg from maturing or being released, leading to irregular or absent ovulation.
- Functional cysts sometimes temporarily disturb the normal hormone balance needed for ovulation.
-
Hormonal Imbalances
- Cysts related to conditions like PCOS often come with elevated androgen levels and insulin resistance.
- This hormonal imbalance can make it harder to conceive and maintain a healthy pregnancy.
-
Ovarian Reserve Damage
- Large cysts or those requiring surgical removal can, in some cases, damage healthy ovarian tissue.
- This can reduce the “ovarian reserve,” which is the number of healthy eggs you have left for future ovulation.
-
Scarring and Structural Problems
- Endometriosis-related cysts (endometriomas) can lead to scarring around the ovaries and fallopian tubes.
- Scarring can hinder the egg’s journey into the uterus, affecting fertilization.
-
Egg Quality Issues
- In endometriosis or severe PCOS, the local environment in the ovary can become inflamed.
- Inflammation or hormone imbalances can affect the eggs’ development and quality.
However, it’s important to note that many ovarian cysts never cause fertility problems and can be monitored through “watchful waiting.” If your doctor thinks a cyst might pose a threat to your fertility, they can recommend treatments that may help prevent further complications.
Symptoms and Warning Signs You Shouldn’t Ignore
Many ovarian cysts are silent—meaning they come and go without notice. However, there are some signs that might suggest you have a cyst, especially if it’s large or causing hormonal changes. Here are the main symptoms and warning signs:
- Pelvic pain or pressure on one side of your lower abdomen
- Bloating or fullness in the belly
- Irregular menstrual cycles (too long, too short, or unpredictable)
- Spotting or abnormal bleeding
- Painful intercourse
- Frequent urination if the cyst is pressing on your bladder
- Sudden, severe abdominal pain (which could mean rupture or torsion—an emergency)
When to See a Doctor
If you experience sudden, sharp pelvic pain that doesn’t go away, or if you notice heavy bleeding with dizziness or weakness, seek medical attention immediately. These could be signs of a ruptured cyst or ovarian torsion, both of which require urgent treatment.
Diagnosing Ovarian Cysts: How Doctors Can Help
If you have any symptoms that suggest an ovarian cyst or you’re worried about your fertility, a doctor can do a few tests to diagnose the problem:
-
Pelvic Examination
- A standard pelvic exam might show an enlarged ovary or tenderness.
-
Transvaginal Ultrasound
- An ultrasound probe is inserted into the vagina for a close-up view of your ovaries.
- This is the most common and reliable way to see the size, shape, and location of a cyst.
-
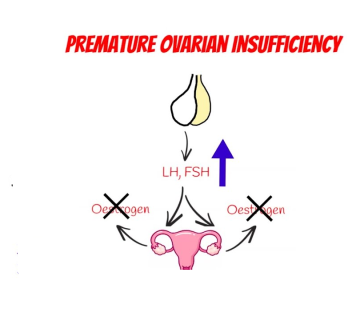
Blood Tests
- Your doctor might check hormone levels (like LH, FSH, testosterone, and progesterone).
- They might also test for CA-125, a tumor marker that can be elevated in certain ovarian cysts, including some cancerous ones and endometriomas.
-
MRI or CT Scan
- Less common but sometimes used if an ultrasound is inconclusive or if there’s a concern about something more serious.
-
Laparoscopy
- A surgical procedure where a small camera (laparoscope) is inserted into the abdomen to view the reproductive organs.
- This is both a diagnostic and potential treatment method because the doctor can remove suspicious cysts during the procedure.
Getting an accurate diagnosis is crucial, especially if you’re trying to conceive. By identifying the type of cyst, doctors can tailor a plan to protect or improve your fertility.
Treatment Options: From “Watchful Waiting” to Surgery
1. Watchful Waiting
For small, simple cysts, especially functional cysts, doctors often take a watchful approach:
- Core point: Many functional cysts disappear on their own after one or two menstrual cycles.
- Practical tip: Schedule follow-up ultrasounds to monitor the cyst’s size and any changes.
2. Medications
- Birth Control Pills: These pills can help prevent new cysts from forming by stopping ovulation. They may also help shrink existing cysts over time.
- Hormonal Therapy: In cases of PCOS or hormonal imbalance, doctors may recommend medications like metformin (for insulin resistance) or others that regulate hormones and support healthy ovulation.
3. Minimally Invasive Procedures
- Laparoscopic Surgery: When a cyst is large, painful, or suspected to be causing fertility issues, a surgeon may remove it via a small incision.
- Draining the Cyst: In rare situations, a doctor might drain fluid from a cyst, but this approach has a higher chance of recurrence compared to removal.
4. Open Surgery (Laparotomy)
If the cyst is unusually large or looks suspicious for cancer, an open surgery might be performed. This involves a larger incision in the abdomen and is usually reserved for more serious cases.
5. Fertility Treatments
- Ovulation Induction: Medications like clomiphene citrate can stimulate ovulation in women with PCOS or other hormonal issues.
- In Vitro Fertilization (IVF): Recommended if you have multiple factors affecting fertility, such as severe endometriosis or a low ovarian reserve.
Can Natural Remedies and Lifestyle Changes Help?
While medical treatment is often necessary for certain kinds of cysts (especially large or complex ones), there are also natural approaches that may be beneficial. Although these aren’t guaranteed cures, they can support hormone balance and overall reproductive health.
Diet: Focus on Whole, Nutrient-Rich Foods
- Fiber-Rich Fruits and Vegetables: Berries, leafy greens, beans
- Lean Proteins: Fish, skinless poultry, beans, lentils
- Healthy Fats: Avocados, olive oil, nuts, seeds
- Low-Glycemic Carbohydrates: Whole grains instead of white bread or pasta
A balanced diet helps regulate insulin and may keep hormone levels in check, which is especially relevant for women with PCOS. In fact, research suggests that weight loss (even 5-10% of total body weight) can restore ovulation in some women with PCOS, increasing their chances of pregnancy.
Exercise: Moderate and Regular
- Core point: Regular exercise helps maintain a healthy weight and regulate hormones.
- Try: At least 30 minutes of moderate exercise (like brisk walking or cycling) 5 times a week.
- Caution: Excessive exercise or intense workouts can sometimes negatively impact menstrual cycles, so aim for balance.
Stress Management
Chronic stress can raise cortisol levels, which can then disrupt other hormones, including those important for reproduction. Activities like yoga, deep breathing, or journaling may help.
Supplements and Herbs
Some women try supplements like vitex (chasteberry), omega-3 fatty acids, or inositol to support reproductive health. While some anecdotal evidence and small studies exist, always talk to a healthcare provider first. Supplements can have side effects or interact with medications.
✔️ Recommended Natural Approaches
- ✔️ Balanced, nutrient-dense meals
- ✔️ Regular, moderate exercise
- ✔️ Adequate sleep (7–8 hours per night)
- ✔️ Managing stress through mindfulness or counseling
❌ What to Avoid
- ❌ Crash diets or extreme caloric restriction
- ❌ High-sugar, high-processed foods
- ❌ Excessive alcohol consumption
- ❌ Smoking (linked to many reproductive issues)
Additional Factors That Influence Fertility
Even if you have an ovarian cyst, your overall fertility picture isn’t limited to that alone. Other factors can play a significant role:
-
Age
- A woman’s fertility generally starts to decline after age 35.
- If you’re in your late 30s or 40s, it’s essential to have a clear plan.
-
Medical History
- Past surgeries, sexually transmitted infections, or conditions like endometriosis can affect fertility.
-
Lifestyle Choices
- Smoking, high alcohol use, and poor diet can lower fertility.
-
Genetics
- Some women are genetically predisposed to conditions like PCOS, endometriosis, or early menopause.
-
Partner’s Health
- Male factor infertility (such as low sperm count or poor sperm quality) might also be part of the fertility equation.
- Always consider both partners’ health when addressing fertility problems.
Minimizing the Risk of Ovarian Cysts: Practical Steps
While not all cysts can be prevented—especially those tied to genetics or chronic conditions—there are ways to lower the chances of developing them or catching them early.
Step-by-Step Guide for Prevention and Early Detection
-
Schedule Regular Check-ups
- Visit your OB-GYN at least once a year for a pelvic exam.
- Discuss any menstrual irregularities or pelvic discomfort right away.
-
Track Your Menstrual Cycle
- Use a calendar or app to monitor regularity, flow, and symptoms.
- Irregularities can be an early sign something’s off.
-
Maintain a Healthy Weight
- Excess body fat can lead to higher estrogen levels, which can encourage certain cysts to form.
- If you’re overweight, aim for gradual weight loss through balanced diet and exercise.
-
Consider Hormonal Birth Control
- If you’re not trying to conceive, certain types of birth control can regulate your cycle and reduce the formation of functional cysts.
-
Limit Exposure to Endocrine Disruptors
- Chemicals like BPA and phthalates (found in some plastics and personal care products) can disturb hormone balance.
- Opt for BPA-free containers and natural skin-care products when possible.
-
Manage Stress
- High stress can worsen hormonal imbalances, especially in conditions like PCOS or endometriosis.
-
Seek Timely Medical Advice
- If you notice any persistent symptoms such as ongoing pain, bloating, or unusual bleeding, see your doctor for an evaluation. Early intervention can prevent complications.
Emotional Impact: Coping With Uncertainty
Finding out you have an ovarian cyst can spark a flurry of emotions—relief if it’s small and harmless, or worry if you’re unsure whether it might affect your dreams of having children. It’s normal to feel stressed or overwhelmed. Consider the following ways to cope:
- Talk to a Professional: A counselor or therapist can help you process fears, especially if fertility is a pressing concern.
- Join Support Groups: Online or in-person communities of women experiencing similar issues can offer emotional backup and practical advice.
- Educate Your Partner: If you’re planning to start a family, involve your partner in discussions and appointments. Shared understanding can ease anxiety.
- Focus on What You Can Control: Lifestyle changes like diet, exercise, and stress management are within your power and can significantly boost your overall reproductive health.
Frequently Asked Questions (FAQ)
1. Can I get pregnant if I have an ovarian cyst?
Yes, you can. Many women with ovarian cysts conceive naturally, especially if the cysts are small and functional. However, it depends on the type and severity of the cyst. Conditions like PCOS or endometriomas can make pregnancy more challenging, but not impossible.
2. Do all ovarian cysts need surgery?
No. Most functional cysts go away on their own. Surgery is generally reserved for cysts that are large, causing painful symptoms, or look suspicious on imaging tests.
3. Will birth control pills cure my cysts?
Birth control pills don’t cure cysts, but they can help prevent new ones from forming. They may also help existing functional cysts shrink by stabilizing hormone levels.
4. How quickly can an ovarian cyst grow?
Growth rates vary. Some cysts grow slowly over months, while others remain small and disappear quickly. If your cyst is growing rapidly, your doctor may want to monitor it more closely or recommend removal.
5. Is it normal to have recurring ovarian cysts?
Yes, especially for women with hormonal imbalances like PCOS. Recurring cysts can also be linked to endometriosis. Regular check-ups and hormone regulation can help manage or reduce the frequency of cyst formation.
6. Are there any new research findings that might help?
New studies frequently look into innovative fertility treatments, less invasive surgical techniques, and better medications for hormonal disorders. For example, improved laparoscopic methods now allow many women to preserve ovarian tissue while removing cysts, thus helping maintain fertility. Always ask your doctor about new options or clinical trials that might benefit your situation.
Addressing Less Discussed Topics: What Else Should You Know?
While most articles cover the main points about ovarian cysts and infertility, there are a few extra considerations that often get overlooked:
-
Impact on Mental Health
- Chronic pelvic pain or worries about fertility can heighten anxiety and depressive symptoms. It’s important to address mental well-being alongside physical health.
-
Post-Surgical Recovery
- If you do need surgery (especially laparotomy), recovery can be significant. You may need to wait a while before trying to conceive. Understanding this ahead of time helps with planning.
-
Fertility Preservation
- In certain cases, freezing eggs (egg cryopreservation) might be worth discussing if you face repeated surgeries or have a condition like endometriosis that could worsen over time.
-
Comprehensive Hormone Panels
- Sometimes, only basic hormone tests are done. Request a full panel to get a deeper look into thyroid hormones, insulin, and other factors that could influence cysts and fertility.
-
Environmental Toxins
- Though less studied, there is growing interest in how chemicals in our environment might affect ovarian health. Seeking out cleaner food, water, and personal care products could have long-term benefits.
By keeping these additional points in mind, you can gain a more holistic view of how to protect your fertility and overall health.
Putting It All Together: Your Roadmap to Better Reproductive Health
-
Identify Symptoms Early
- If you notice changes in your menstrual cycle, persistent pelvic pain, or unusual bloating, don’t ignore them. Early detection of ovarian cysts can save you from complications down the road.
-
Talk to Your Doctor
- Open communication ensures personalized advice. Ask about the size, type, and potential risks of your cyst. Discuss all treatment options, including watchful waiting.
-
Consider a Multi-Disciplinary Team
- Working with a gynecologist, endocrinologist, nutritionist, and mental health counselor can address multiple aspects of your well-being.
-
Adopt a Healthy Lifestyle
- Balanced nutrition, regular exercise, and stress management can help prevent or minimize certain types of cysts, support normal ovulation, and increase your chances of conceiving.
-
Stay Informed
- Medical knowledge evolves, and new treatments for ovarian cysts and infertility are emerging. Keep asking questions, reading reputable sources, and seeking second opinions if necessary.
Your Fertility Action Plan: Dos and Don’ts
Here’s a quick checklist to guide you in managing ovarian cysts and optimizing fertility:
✔️ DO:
- ✔️ Schedule regular pelvic exams and ultrasounds
- ✔️ Maintain a healthy weight
- ✔️ Manage stress through mindfulness or therapy
- ✔️ Ask about hormone therapy or fertility treatments if needed
- ✔️ Keep track of your menstrual cycles
❌ DON’T:
- ❌ Self-diagnose or ignore persistent symptoms
- ❌ Start herbal supplements without professional guidance
- ❌ Rely on internet rumors; confirm with a medical provider
- ❌ Skip follow-up appointments
- ❌ Overdo intense workouts or restrictive diets
Interact With Us!
We’d love to hear from you. Have you or someone you know dealt with ovarian cysts while trying to get pregnant? What strategies helped you the most—medical treatments, lifestyle changes, or emotional support? Your experiences can inspire and inform others on this journey.
Feel free to leave a comment or ask a question about anything covered in this article. We value your insights! By sharing, you might help someone who’s going through the same concerns and searching for guidance.
Thank you for reading this in-depth guide on ovarian cysts and their impact on fertility. We hope you found the information clear, helpful, and empowering. Remember, if you suspect you have an ovarian cyst or are facing difficulty conceiving, professional medical advice is always the best course of action. Stay informed, proactive, and positive—you’ve got this!
No comment