Does Testosterone Lower Sperm Count?
Many men wonder whether boosting testosterone levels might harm their fertility. It’s an important concern, especially for couples trying to conceive. After all, testosterone is a key male hormone involved in sex drive, muscle mass, and energy levels—but does taking extra testosterone from outside sources actually reduce sperm count?
In this in-depth article, we’ll explore how testosterone works in the body, why sperm production depends on it, and what happens when you use testosterone therapy or other methods to raise testosterone levels. We’ll dig into the science, share recent research findings, and offer practical tips to help you make informed decisions about your reproductive health. By the end, you’ll have a clear understanding of how testosterone and sperm count are linked, and what you can do to protect or improve your fertility.
What Is Testosterone?
Core Idea
Testosterone is a hormone produced mostly in a man’s testicles. It plays a huge role in:
- Building muscle mass and strength
- Maintaining bone density
- Controlling sex drive (libido)
- Aiding sperm production
- Influencing mood and energy levels
Small amounts of testosterone are also made by a woman’s ovaries and adrenal glands, but men typically have much higher levels.
Detailed Explanation
For men, the hypothalamus in the brain signals the pituitary gland to release hormones (Luteinizing Hormone, LH, and Follicle-Stimulating Hormone, FSH). LH prompts the testicles to produce testosterone, while FSH helps stimulate sperm production. Testosterone then circulates through the bloodstream, influencing many parts of the body.
But here’s a twist: if you introduce extra testosterone into your body—often called exogenous testosterone—the body senses these higher levels. Your hypothalamus and pituitary gland might reduce or shut down their signals (LH and FSH) because they think you already have enough. That can lead to lower natural testosterone production and reduced sperm production. This is why there’s a connection between taking outside testosterone and a drop in sperm count.
Scientific Support
- Research has shown that men who receive testosterone replacement therapy (TRT) often experience a decrease in sperm concentration and overall sperm count.
- Studies in reputable journals (e.g., Journal of Urology, Fertility and Sterility) confirm that blocking the body’s natural production signals can temporarily or sometimes more persistently reduce fertility.
Practical Tip
If you’re considering testosterone therapy, talk to a knowledgeable healthcare provider about how it might affect your fertility. There may be ways to manage or minimize potential negative effects on sperm production, such as using medications like hCG (human chorionic gonadotropin) that can help keep natural production signals active.
Understanding Sperm Production
Core Idea
Sperm production is a finely tuned process that involves multiple steps in the male reproductive system, guided largely by hormones like testosterone, FSH, and LH.
Detailed Explanation
Inside the testicles, there are tiny tubes called seminiferous tubules. These tubules are where sperm cells grow and mature. The body needs healthy levels of testosterone and FSH to ensure these cells develop properly. If either hormone is too low, sperm production can drop, leading to a lower sperm count or poor sperm quality.
At the same time, too much external testosterone can confuse the body’s hormone-regulating system. Think of it like a thermostat that shuts off when the temperature gets too high—your brain will send fewer signals to produce testosterone and sperm because it senses that your hormone “thermostat” has reached a high reading.
Research Highlights
- A study published in the American Journal of Men’s Health found that men with normal hormone levels who started using testosterone injections saw a decline in FSH, which is crucial for sperm development.
- Another paper in Reproductive Biology and Endocrinology confirmed the direct link between suppressed FSH levels and reduced sperm count among men on exogenous testosterone.
Practical Tip
Routine hormone testing can help you understand if your testosterone, LH, and FSH levels are balanced. If you have unexplained fertility issues or symptoms of low testosterone, testing is a great first step before pursuing any therapy.
The Feedback Loop: Why Outside Testosterone Can Lower Fertility
Core Idea
Hormones operate in a feedback loop involving the hypothalamus, pituitary gland, and testicles—often referred to as the Hypothalamic-Pituitary-Gonadal (HPG) axis. Outside testosterone can disrupt this loop.
The Loop in Simple Terms
- Hypothalamus releases Gonadotropin-Releasing Hormone (GnRH).
- Pituitary Gland detects GnRH and releases LH and FSH.
- Testicles respond to LH by producing testosterone; they respond to FSH by producing sperm.
When you add extra testosterone from an injection, gel, or pellet, your hypothalamus may reduce or stop GnRH release. With less GnRH, your pituitary gland releases less LH and FSH, which are crucial for sperm production.
Research Highlights
- Several studies show that after 3 to 6 months on TRT, men can see significant declines in sperm count. Some experience near-zero sperm count (azoospermia). However, sperm production often recovers if therapy is stopped, though recovery can take months or even over a year in some cases.
- Modern fertility clinics emphasize the importance of addressing this feedback loop when prescribing testosterone to men who still desire children.
Practical Tips
- ✔️ Consider alternative treatments such as Clomiphene Citrate or hCG to stimulate the body’s own testosterone production without halting sperm creation.
- ❌ Avoid self-prescribing or using “black market” testosterone, which can lead to unmonitored hormone imbalances and fertility problems.
- ✔️ Talk with a fertility specialist if fatherhood is a priority and you also have low testosterone symptoms.
Does Testosterone Replacement Therapy (TRT) Always Lower Sperm Count?
Core Idea
Not every man will experience a drastic drop in fertility, but there is a strong likelihood that sperm count will go down to some extent while on TRT. The severity can depend on dosage, duration, and individual body chemistry.
Detailed Explanation
- Short-Term Use: Some men might not see huge changes right away, especially if the dose is moderate or if they use certain adjunct medications.
- Long-Term Use: Prolonged therapy can lead to a more profound suppression of natural testosterone and sperm production.
- Individual Differences: Genetics, lifestyle habits, and existing health conditions can influence how the body responds to added testosterone.
Study Findings
A review in the journal Human Reproduction Update noted that while most men see a marked decrease in sperm production during TRT, the effects can be reversed by stopping therapy. Roughly 90% of men will recover normal sperm counts within a year, though this varies widely.
Practical Tip
If you’re on TRT and hoping to conceive, work with an endocrinologist or fertility specialist to monitor hormone levels and sperm parameters. They may adjust the dosage or add supportive treatments.
Testosterone Boosters vs. TRT
Core Idea
There’s a difference between prescription testosterone replacement therapy (like injections, patches, or pellets) and over-the-counter “testosterone boosters” made from herbs, vitamins, or other supplements. However, each can still impact fertility in different ways.
Detailed Explanation
- Prescription TRT: Typically uses synthetic testosterone to replace what your body isn’t producing enough of. It’s regulated, doctor-prescribed, and potent.
- Over-the-Counter Boosters: Often contain herbal extracts (like fenugreek, ashwagandha, or tribulus terrestris) and nutrients (zinc, vitamin D, etc.) that claim to support the body’s natural testosterone production.
- Are Boosters Safe for Fertility? There’s limited scientific evidence showing that these boosters significantly raise T levels enough to cause big changes in sperm count. However, some supplements might not be well-studied, and certain ingredients could have hormonal effects.
Quick Checklist
- ✔️ Fenugreek: May slightly improve libido and energy, with uncertain effects on sperm.
- ❌ Unregulated “Testosterone” Products: Risk of contamination with actual steroids, which can harm fertility.
- ✔️ Balanced Nutrition: Adequate protein, vitamins, and minerals can support overall hormone health.
Practical Tip
Before trying any T-boosting supplement, research its ingredients and check reputable sources. Some men prefer to focus on diet, exercise, and sleep first, as these natural methods can help improve hormone balance without risking a major drop in sperm production.
Signs of Low Testosterone: Could It Be Something Else?
Core Idea
Sometimes men jump to testosterone therapy without confirming if they truly have low T. Low energy, low libido, and other symptoms can also result from stress, poor sleep, depression, or other medical conditions.
Detailed Explanation
-
Common Symptoms of Low T:
- Reduced sex drive and erectile issues
- Fatigue and poor energy levels
- Loss of muscle mass or increased body fat
- Mood swings or depression
- Difficulty concentrating
-
Other Possible Causes:
- Thyroid disorders can mimic low T symptoms.
- Vitamin D deficiency can cause low energy and mood changes.
- High stress or poor sleep can lower testosterone over time.
Scientific Insight
A study in the Journal of Clinical Endocrinology & Metabolism found that many men with borderline testosterone levels improved after addressing obesity, improving diet, and increasing physical activity—no TRT needed.
Practical Steps
- Get a thorough check-up including blood tests for thyroid function, vitamin levels, and hormone panels.
- Try lifestyle modifications like weight loss or better sleep before jumping into TRT.
- Talk to a therapist or counselor if stress or mental health issues are significant.
Lifestyle Factors Affecting Testosterone and Fertility
Core Idea
Lifestyle plays a major role in both testosterone levels and sperm count. Even small changes can have a positive impact.
Detailed Explanation
-
Diet
- Healthy fats (avocados, nuts, olive oil) help hormone production.
- Lean protein supports muscle growth.
- Excess sugar and processed foods can contribute to weight gain, which negatively affects T levels.
-
Exercise
- Weightlifting or resistance training is known to boost T levels.
- High-intensity interval training (HIIT) can also help, as it challenges the body in short bursts.
- Excessive endurance training (like very long-distance running) may lower T in some men.
-
Sleep
- 7 to 9 hours of quality sleep each night helps maintain healthy hormone cycles.
- Chronic sleep deprivation can lead to lower testosterone and reduced sperm quality.
-
Stress Management
- Chronic stress increases cortisol, which can reduce testosterone and harm sperm development.
- Activities like yoga, meditation, or hobbies can help manage stress levels.
-
Avoiding Toxins
- Smoking can decrease sperm quality.
- Excessive alcohol consumption can also lower testosterone and affect sperm health.
- Drugs or anabolic steroids have a strong negative impact on fertility.
Checklist: Lifestyle Do’s and Don’ts
✔️ DO
- Eat a balanced diet with whole foods
- Incorporate regular resistance training
- Prioritize 7–9 hours of sleep
- Practice stress reduction (deep breathing, hobbies, mindfulness)
❌ DON’T
- Overindulge in alcohol or tobacco
- Neglect sleep or live with chronic stress
- Rely solely on supplements without broader lifestyle improvements
- Skip regular medical check-ups
Recent Research & Emerging Therapies
Core Idea
Science continues to evolve in understanding how best to treat low testosterone without harming fertility. Some newer approaches focus on stimulating the body’s natural hormone production rather than replacing testosterone outright.
Emerging Treatments
-
Clomiphene Citrate (Clomid)
- Acts on the pituitary gland to increase LH and FSH, thus boosting natural testosterone production and maintaining sperm count.
- Often prescribed to men who want to improve T levels but also maintain fertility.
-
Enclomiphene
- A selective estrogen receptor modulator (SERM), similar to Clomid but more targeted.
- Can raise T levels while preserving or even enhancing sperm production in some cases.
- Still being researched, but some fertility clinics already use it off-label.
-
hCG (Human Chorionic Gonadotropin)
- Mimics LH in the body, promoting testosterone production in the testicles.
- Often used alongside TRT to keep testicular function more active, potentially preserving sperm count.
Research Highlights
- A 2022 study in Frontiers in Endocrinology discussed the effectiveness of Clomiphene Citrate in men with secondary hypogonadism, showing improvement in both T levels and sperm parameters.
- A recent trial on enclomiphene showed promising results in maintaining sperm counts in men with mild to moderate low T, though more large-scale studies are needed.
Practical Tip
Ask your doctor about these newer methods if you’re concerned about fertility. They can be a more “fertility-friendly” approach than standard testosterone injections or gels alone.
Can You Raise Testosterone Naturally Without Lowering Sperm Count?
Core Idea
Yes! There are several natural strategies that can help you optimize hormone levels and possibly enhance fertility at the same time.
Detailed Explanation
-
Weight Loss
- Excess body fat can boost estrogen levels and reduce testosterone. Losing weight if you’re overweight can help restore hormonal balance.
-
Nutrient-Rich Diet
- Include foods high in zinc (oysters, pumpkin seeds), selenium (brazil nuts, fish), and vitamin D (salmon, fortified milk, sunlight exposure).
- These nutrients support healthy sperm and testosterone production.
-
Exercise & Muscle Building
- Resistance training 3-4 times a week can naturally stimulate T production.
- Avoid overtraining, which can stress the body and lower T levels over time.
-
Stress Reduction
- Chronic stress leads to high cortisol, which negatively impacts testosterone.
- Meditation, regular breaks, or even short walks can help keep stress in check.
-
Quality Sleep
- Testosterone is produced mainly during deep sleep. Aim for at least 7 hours to help maintain hormone balance.
Evidence
- Weight loss: A study in Obesity Research & Clinical Practice found that obese men who lost an average of 10% of their body weight saw a measurable increase in testosterone levels.
- Diet & Nutrients: Research in Fertility and Sterility linked higher zinc intake to improved sperm parameters.
- Sleep: A study at the University of Chicago showed men who slept less than 5 hours a night over a week had significant drops in daytime testosterone levels.
Practical Tip
Try a 90-day lifestyle experiment: Focus on a balanced diet, consistent sleep schedule, regular workouts, and stress management. Track how you feel, and consider retesting your hormone levels afterward.
Balancing Testosterone Therapy With Fertility Goals
Core Idea
If you truly need testosterone therapy for symptomatic low T but still want children, a careful plan can help you achieve both.
Potential Strategies
-
Short-Term TRT With hCG
- Adding hCG may help maintain testicular stimulation, reducing negative impacts on sperm production.
-
Clomid or Enclomiphene First
- These medications might boost T levels enough without drastically lowering sperm count.
-
Fertility Preservation
- Consider sperm banking before starting TRT if you have no immediate fertility plans but might want children in the future.
-
Frequent Monitoring
- Regular semen analyses can help you stay on top of any changes in sperm health.
- Hormone blood tests can guide dosage adjustments.
Table: Comparison of Fertility-Friendly Options
| Approach | Main Benefit | Potential Drawback | Best For |
|---|---|---|---|
| TRT + hCG | Maintains some testicular function | May be more complex/expensive | Men with diagnosed hypogonadism who want kids |
| Clomiphene/Enclomiphene | Boosts body’s own T production | Not effective for all; side effects vary | Men with mild to moderate low T, fertility needs |
| Sperm Banking | Ensures future fertility option | Additional cost; requires lab storage | Men uncertain about timing for fatherhood |
| Lifestyle Changes | Improves overall health | Takes time and discipline | Men with borderline or slight low T |
Practical Tip
Always discuss your plan with a doctor who understands both endocrinology and reproductive health. This may mean seeking out an endocrinologist and a fertility specialist working together.
What If You’ve Already Used Testosterone and Now Want Kids?
Core Idea
It’s common to worry that past or current testosterone use may have harmed your long-term fertility. The good news is that for most men, sperm count can recover if the therapy is stopped or adjusted.
Detailed Explanation
-
Stopping Exogenous Testosterone
- This removes the negative feedback on the HPG axis, allowing your body to start producing LH and FSH again.
- Recovery times vary. Some men see improvement in 3 months, others may need 12+ months to get back to normal sperm levels.
-
Adding Supportive Medications
- A doctor might prescribe hCG or Clomiphene to jumpstart your system.
- Regular testing will track your progress.
-
Lifestyle Optimizations
- Focus on diet, exercise, sleep, and stress management to help speed up recovery.
- Avoid substances like alcohol, tobacco, and other drugs that could slow or block hormone restoration.
-
Fertility Testing
- Consider doing a semen analysis to measure sperm count, motility, and morphology.
- Hormone blood tests (LH, FSH, total testosterone, etc.) can confirm whether levels are returning to normal.
Practical Tip
Patience is key. If you’ve used testosterone for a while, you might need many months to see a strong return of fertility. Keep close communication with your healthcare provider and track your progress.
Additional Factors Affecting Male Fertility
Core Idea
Beyond testosterone, several other factors can influence your ability to conceive.
Common Influencers
-
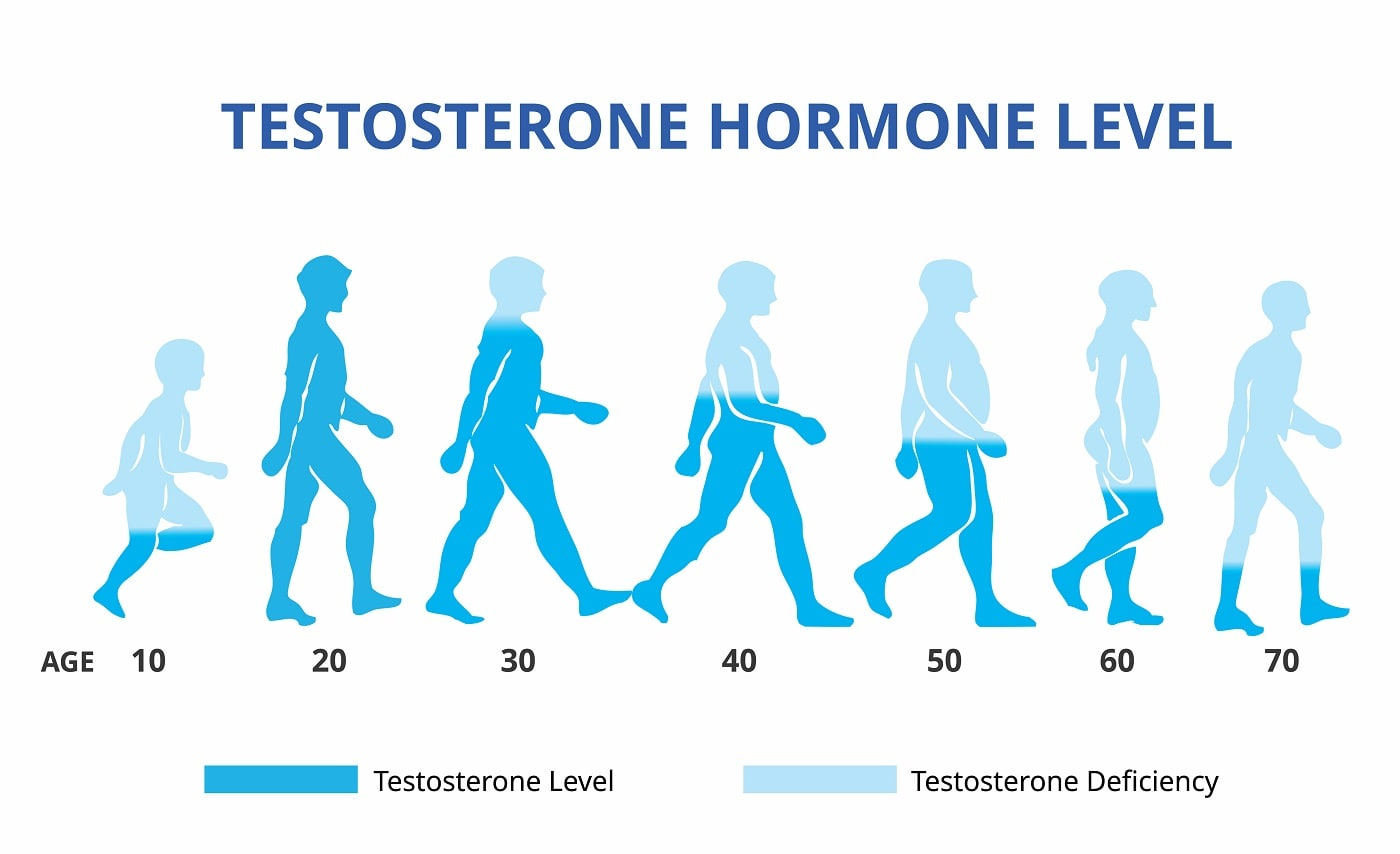
Age
- Sperm quality can gradually decline as men get older, although it remains possible to father children well into later years.
-
Genetics
- Some men have genetic conditions (like Klinefelter syndrome) that lower fertility regardless of T levels.
-
Varicocele
- Enlarged veins in the scrotum can overheat the testicles, negatively affecting sperm production.
-
Medications
- Certain drugs for blood pressure, depression, or chemotherapy can affect fertility.
- Always tell your doctor about all medications and supplements you use.
-
Environmental Exposure
- Chemicals like pesticides or toxins in the workplace can impact sperm health.
- Wearing tight underwear or exposure to excessive heat (like hot tubs) may also lower sperm quality over time.
Practical Tip
When facing fertility challenges, it’s best to look at your health from all angles. A thorough check-up can help spot issues unrelated to testosterone but still affecting sperm count.
Myths and Misconceptions
Core Idea
Testosterone and fertility are surrounded by myths. Let’s clear up some common misconceptions so you can make better decisions.
Common Myths vs. Facts
-
Myth: “Testosterone therapy always makes you feel better immediately.”
- Fact: Some men do feel improvements in energy or libido, but it can take weeks to notice real benefits. Sperm production can still drop in the meantime.
-
Myth: “Taking extra testosterone is the best way to get big muscles quickly.”
- Fact: While anabolic steroids or high-dose testosterone can increase muscle mass, they can also severely shut down sperm production, not to mention other health risks.
-
Myth: “Over-the-counter testosterone boosters have zero effect on fertility.”
- Fact: Some OTC products are spiked with actual hormones or untested chemicals. These can impact fertility in unpredictable ways.
-
Myth: “Once you ruin your fertility with testosterone, there’s no going back.”
- Fact: Most men recover sperm production after stopping TRT, though it can take time and sometimes medical support.
-
Myth: “Low libido always means low T.”
- Fact: Libido can be influenced by stress, relationship factors, mental health, medications, and more. Low T is just one possible cause.
Practical Tip
Focus on science-based information. If you see wild claims about “doubling your testosterone overnight” or “instant muscle gains,” it’s a red flag. Reputable medical advice is your safest bet.
Step-by-Step Guide to Protecting Your Fertility While Managing Testosterone
Core Idea
For men balancing their desire for children with the need for healthy testosterone levels, a proactive approach can make all the difference.
Steps to Follow
-
Consult Professionals
- Schedule an appointment with a urologist or endocrinologist specializing in male fertility.
- Discuss any low T symptoms, past testosterone use, and future family planning goals.
-
Get a Comprehensive Hormone Panel
- LH, FSH, Total Testosterone, Free Testosterone, and Estradiol levels provide a detailed picture.
- If needed, also check thyroid function, prolactin, and vitamin D.
-
Assess Semen Quality
- A semen analysis measures sperm count, motility, and morphology.
- Repeat this test every few months if you’re actively trying to conceive or adjusting hormone therapies.
-
Evaluate Treatment Options
- Discuss TRT vs. Clomid vs. Enclomiphene vs. hCG with your doctor.
- Weigh the pros and cons of each approach for your unique situation.
-
Optimize Lifestyle
- Weight Management: Achieve or maintain a healthy BMI.
- Exercise: Aim for regular resistance training, limit excessive cardio if it’s too intense.
- Nutrition: Eat whole foods, focus on protein and micronutrients, limit processed sugars.
- Sleep & Stress: Improve sleep hygiene, practice relaxation techniques.
-
Monitor and Adjust
- Regular blood tests to monitor hormone levels.
- Repeat semen analyses to see how sperm count reacts.
- Adjust medication dosages or switch therapies as needed.
-
Consider Sperm Banking
- If you plan on being on TRT long-term or using it at higher doses, sperm banking can be an “insurance policy” against unexpected fertility declines.
Practical Tip
Document everything in a personal health journal: track daily habits, energy levels, changes in workout performance, or any side effects. This helps you and your doctor spot trends and make timely adjustments.
Real-Life Example: Balancing TRT and Fatherhood
Core Idea
A short story or example can help highlight how someone might juggle testosterone therapy with fertility goals.
James, Age 32
- James has struggled with low energy, low libido, and moderate depression. After blood tests, doctors diagnose him with low testosterone levels. He’s also newly married and wants kids in the next year or two.
- His doctor suggests sperm banking before starting TRT, and includes hCG in his treatment plan to maintain testicular function. They agree to do regular blood tests and semen analyses every three months.
- Over time, James notices improved mood and energy from TRT but also sees his sperm count drop a bit. Because he banked sperm earlier, he feels less stressed. His doctor eventually switches him to a lower TRT dose and adjusts hCG, which helps maintain a workable sperm count.
- After about six months, James and his wife start trying to conceive. With the help of these careful adjustments and his stored sperm as a backup, James feels confident about his fertility future.
Beyond Testosterone: Holistic Approaches to Male Reproductive Health
Core Idea
When we talk about male fertility, testosterone is just one piece of the puzzle. A holistic approach can often yield better long-term results.
Holistic Methods
-
Mind-Body Techniques
- Yoga can improve flexibility, reduce stress hormones, and enhance overall circulation.
- Meditation and breathing exercises can keep cortisol levels in check, helping hormone balance.
-
Nutritional Counseling
- Working with a dietitian ensures your diet is aligned with fertility goals (e.g., enough antioxidants, healthy fats, minimal processed foods).
-
Address Relationship Health
- Emotional stress or tension with a partner can indirectly affect libido and sperm production.
- Counseling or open communication can help reduce stress and keep intimacy positive.
-
Check for Vitamin & Mineral Deficiencies
- Zinc, Vitamin D, Magnesium are crucial for hormone health.
- Blood tests can reveal hidden deficiencies that might be dragging your levels down.
-
Routine Medical Screenings
- Ensure routine testicular exams to catch issues like varicocele early.
- Monitoring blood pressure, cholesterol, and diabetes risk factors is important for overall health, which in turn affects reproductive health.
Practical Tip
A balanced life—physically, mentally, and emotionally—is key to strong fertility. Even if you take medical treatments, ignoring overall wellness can undermine your efforts.
Frequently Asked Questions
Q: If I use testosterone injections for a short time, will my sperm count definitely drop?
A: Most men do see some drop in sperm count, but “how much” varies. Short-term use may produce only a mild decrease, and fertility often returns after discontinuing. Always monitor your levels if you’re concerned.
Q: Are “natural testosterone boosters” safe for fertility?
A: Some herbal formulas may be safe, but they’re often not well-regulated. They might not raise testosterone enough to harm sperm significantly, but contamination or unknown interactions are a risk. Check labels and choose reputable brands.
Q: Can I still build muscle naturally with low T?
A: Yes, you can still improve muscle mass through proper weight training, nutrition, and sleep. However, severely low T might make gains slower. Treating the underlying cause of low T (e.g., obesity, lack of sleep) can help.
Q: How long does it take for sperm count to return to normal after stopping TRT?
A: It varies widely—some men recover within 3–6 months, while others may need 12–18 months. Underlying health factors and the duration of TRT use matter a lot.
Q: Could I freeze sperm before starting TRT?
A: Yes, sperm banking is a common strategy. It offers peace of mind if fertility doesn’t fully rebound later. Discuss this option with your doctor or a fertility clinic.
Bringing It All Together
As you can see, testosterone and sperm count share a delicate relationship. Yes, using outside testosterone can lower sperm production—often significantly—by disrupting the body’s natural hormone signals. However, there are ways to preserve or restore fertility. From lifestyle adjustments and holistic methods to newer fertility-friendly medications, you have options.
The best strategy depends on your unique situation. Are you officially diagnosed with low T? Do you plan on having children soon? Have you tried natural fixes like improved diet, exercise, and sleep? A thoughtful, medically supervised plan can help you achieve healthier testosterone levels without permanently sacrificing your ability to become a father.
Final Thoughts & Your Turn
Before you go, we’d love to hear from you. Let’s keep the conversation going!
- Do you have any personal strategies or experiences managing low T while maintaining fertility?
- What’s one lifestyle change you’re most interested in trying?
- Any unique tips or advice you’d like to share with others facing the same concerns?
Share your thoughts in the comments below. Your insights might help someone else who’s on the same journey. Remember, taking control of your health is an ongoing process—stay curious, ask questions, and work closely with qualified healthcare providers to find what’s right for you.
Disclaimer: This article is for educational purposes only. It does not replace professional medical advice. Always consult a healthcare professional for personalized diagnosis and treatment.