Introduction
Abnormal follicle development can be a major hurdle for anyone dealing with fertility issues. Whether you are just beginning to explore your options or you have been on this journey for a while, understanding the details of this condition is key to finding a solution. In our story, we share how our team tackled a complex case of abnormal follicle development and helped our patient move forward with renewed hope.
In this article, you will learn:
- What abnormal follicle development is and why it matters
- How our team identified the problem with careful testing and evaluations
- The detailed treatment plan that made a difference
- Practical tips and advice for managing similar challenges
- Scientific research and real-life success stories that offer support and encouragement
Our aim is to provide a complete, easy-to-understand guide that answers your questions and gives you practical help. Let’s start by looking at the basics.
Understanding Abnormal Follicle Development
What Are Follicles?
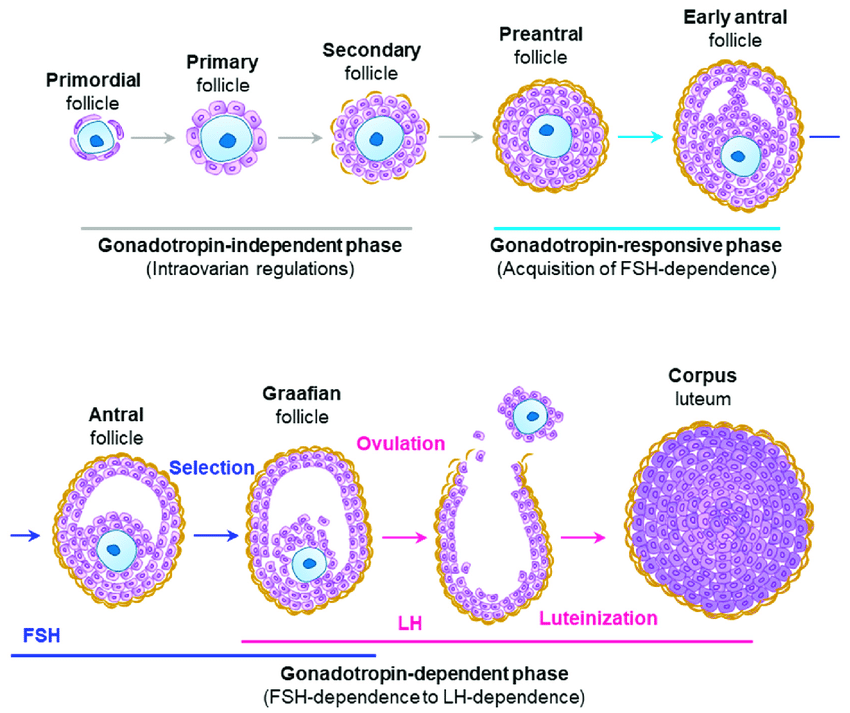
In a woman’s ovaries, follicles are small sacs that hold the eggs. Each month, a group of these follicles begins to grow, and one or more may mature enough for ovulation. Follicles are important because they are the starting point for a potential pregnancy. When everything goes as planned, the egg from the dominant follicle is released and can be fertilized.
Key Points:
- Follicles are like tiny “containers” in the ovaries.
- They hold the eggs and help them grow.
- Healthy follicle development is critical for a regular menstrual cycle and fertility.
What Does Abnormal Follicle Development Mean?
When we talk about abnormal follicle development, we refer to a situation where the follicles do not grow or function as expected. This could mean:
- Delayed or irregular growth: Follicles might not develop at the right time or grow too slowly.
- Poor quality eggs: The eggs inside the follicles might not be healthy.
- Overgrowth or undergrowth: Some follicles might grow too large or fail to grow at all.
These abnormalities can affect fertility by reducing the chances of a healthy egg being available for fertilization.
Common Symptoms and Concerns
Women experiencing abnormal follicle development might notice a range of symptoms, such as:
- Irregular menstrual cycles
- Pain or discomfort in the lower abdomen
- Hormonal imbalances
- Infertility or difficulty conceiving
These symptoms can be both physically and emotionally challenging. It is important to recognize these signs early and seek help from a qualified fertility specialist.
Checklist: Symptoms to Watch For
✔️ Irregular periods
✔️ Abdominal pain or discomfort
✔️ Unexplained hormonal changes
✔️ Trouble getting pregnant
❌ Normal, regular cycles with no issues
The Complex Case: An Overview
Background of the Case
Let’s dive into the story of one complex case of abnormal follicle development. Our patient, whom we will call “Emily” for privacy, had been trying to conceive for several years without success. Emily experienced irregular cycles and occasional pain, but the root cause was unclear. After undergoing a series of tests and evaluations, we discovered that her follicles were not developing as they should. This was a clear sign of abnormal follicle development, which required a deeper look and a customized treatment plan.
Challenges Faced
Every case of abnormal follicle development is unique, and Emily’s case was especially complex. Here are some of the challenges we encountered:
- Irregular Growth Patterns: Emily’s follicles did not follow a predictable growth pattern, making it hard to pinpoint the best time for treatment.
- Hormonal Imbalances: Her hormone levels were not within the normal range, contributing to the irregular development.
- Emotional Stress: Like many patients facing fertility issues, the emotional toll of repeated disappointments was significant.
- Lack of Immediate Solutions: Standard treatments did not work right away, requiring a more detailed, patient-specific approach.
Challenges in Complex Cases
| Challenge | Description | Impact on Treatment |
|---|---|---|
| Irregular Growth Patterns | Follicles did not develop consistently | Difficult to time interventions |
| Hormonal Imbalances | Abnormal hormone levels disrupt normal growth cycles | Complicates treatment planning |
| Emotional Stress | High levels of stress and anxiety | Affects overall health and response to treatment |
| Standard Treatments Unsuccessful | Conventional methods did not yield desired results | Need for customized approach |
Our Approach: How We Helped
Step-by-Step Diagnosis Process
Our first priority was to understand the full scope of Emily’s condition. We used a step-by-step approach to diagnose the issue:
- Detailed Medical History: We reviewed her menstrual history, previous treatments, and lifestyle factors.
- Ultrasound Examinations: Multiple ultrasounds helped us visualize the follicles and their growth patterns.
- Hormone Testing: Blood tests measured levels of key hormones like estrogen, FSH (follicle-stimulating hormone), and LH (luteinizing hormone).
- Additional Imaging: In some cases, further imaging tests, such as MRI, can provide more details about ovarian structure.
Step-by-Step Guide: Diagnostic Process
- Step 1: Gather detailed history and symptoms.
- Step 2: Perform ultrasound to observe follicle development.
- Step 3: Conduct hormone tests to check for imbalances.
- Step 4: Use additional imaging if necessary.
This thorough diagnostic process helped us clearly see the patterns and problems in Emily’s follicle development.
Tests and Evaluations
Our evaluations were not limited to just one test. We combined various tests to create a full picture of the problem. Here’s a brief look at the tests we used:
- Ultrasound: To monitor follicle size and growth over the cycle.
- Blood Hormone Tests: To check levels of estrogen, FSH, LH, and progesterone.
- Genetic Screening: In rare cases, genetic tests may be used to rule out inherited conditions.
- Lifestyle and Diet Review: Sometimes, factors like stress or diet can influence follicle development.
Table: Diagnostic Tests Overview
| Test Type | Purpose | What It Shows |
|---|---|---|
| Ultrasound | Visualize follicle size and number | Growth patterns and abnormalities |
| Blood Hormone Tests | Measure levels of reproductive hormones | Hormonal imbalances, potential causes |
| Genetic Screening | Rule out genetic factors | Inherited conditions affecting follicles |
| Lifestyle & Diet Review | Understand external factors affecting health | Influence of nutrition and stress |
Creating a Personalized Treatment Plan
After gathering all the necessary data, we worked with Emily to design a treatment plan that was tailored specifically to her needs. Our plan included both medical treatments and lifestyle modifications.
Key Points in the Treatment Plan:
- Individualized Approach: Recognizing that each case is unique, we tailored the treatment to address Emily’s specific challenges.
- Combination of Therapies: We combined medication, lifestyle changes, and regular monitoring.
- Regular Follow-Up: Continuous monitoring allowed us to adjust the treatment plan as needed for the best outcome.
Detailed Breakdown of the Treatment
Medications and Lifestyle Adjustments
One of the main parts of our treatment was a carefully chosen medication regimen paired with practical lifestyle changes.
Medications
We prescribed medications designed to stimulate normal follicle growth and correct hormonal imbalances. These might include:
- Gonadotropins: Hormones that help stimulate the ovaries to develop multiple follicles.
- Clomiphene Citrate: A medication that can help trigger ovulation.
- Hormonal Supplements: To balance estrogen and progesterone levels.
Checklist: Medication Benefits and Considerations
✔️ Helps regulate follicle growth
✔️ Can improve hormone balance
❌ Overuse without monitoring may lead to side effects
Lifestyle Adjustments
Along with medication, we advised Emily on lifestyle changes that could support her treatment:
- Diet: Incorporating foods rich in antioxidants and omega-3 fatty acids to improve overall reproductive health.
- Exercise: Moderate exercise to reduce stress and improve blood circulation.
- Stress Management: Techniques such as yoga, meditation, and counseling to help manage emotional stress.
Checklist: Lifestyle Tips ✔️ Eat a balanced, nutritious diet
✔️ Engage in regular, moderate exercise
✔️ Practice stress-relief techniques
❌ Extreme diets or overexercising, which may add stress
Surgical and Non-Surgical Interventions
In some cases, if medications and lifestyle changes are not enough, surgical interventions may be considered. For Emily’s case, our approach was mostly non-surgical, but we always keep surgical options in mind if needed.
Non-Surgical Options:
- Medical Management: Adjusting medication dosages and timings based on regular monitoring.
- Holistic Therapies: Acupuncture and massage therapy to improve blood flow and reduce stress.
Surgical Options (When Needed):
- Laparoscopy: A minimally invasive procedure to inspect the ovaries and correct any structural issues.
- Ovarian Drilling: A treatment sometimes used in cases of polycystic ovary syndrome (PCOS), which can also affect follicle development.
Table: Intervention Options
| Intervention Type | Description | When to Consider |
|---|---|---|
| Medical Management | Adjusting medication and hormone treatments | When irregular growth is due to hormonal imbalance |
| Holistic Therapies | Acupuncture, massage, and counseling | To reduce stress and support overall health |
| Laparoscopy | Minimally invasive surgery to inspect and treat ovaries | Structural issues affecting follicle growth |
| Ovarian Drilling | A procedure to reduce overactive ovarian tissue (in PCOS) | Specific cases where PCOS is involved |
Monitoring and Follow-Up Care
Once the treatment plan was in place, regular monitoring was key to success. Emily attended frequent follow-up appointments, during which we:
- Repeated Ultrasounds: To track follicle growth and make sure the treatment was effective.
- Blood Tests: To keep an eye on hormone levels.
- Consultations: To adjust her treatment plan based on progress and feedback.
Step-by-Step Guide: Monitoring Progress
- Schedule Regular Appointments: Weekly or bi-weekly check-ups during the treatment cycle.
- Perform Follow-Up Ultrasounds: Compare follicle growth with previous results.
- Adjust Medications as Needed: Fine-tune dosages based on test results.
- Keep a Health Diary: Note any changes, side effects, or improvements.
Scientific Research and Support
Latest Studies on Abnormal Follicle Development
Recent research has provided deeper insights into abnormal follicle development. Studies have looked into:
- Hormonal Influences: How imbalances in hormones like FSH, LH, and estrogen affect follicle growth.
- Genetic Factors: Research into genetic markers that might predict abnormal follicle development.
- Lifestyle and Environmental Impacts: How diet, stress, and environmental toxins can play a role.
For instance, one study found that adjusting hormone levels with targeted medications significantly improved follicle development in patients with irregular cycles. Other research has shown that lifestyle interventions, including diet changes and stress reduction, can have a measurable positive impact on ovarian health.
What the Research Says
Scientific Support:
✔️ Hormonal Regulation: Studies confirm that proper management of hormone levels can help normalize follicle growth.
✔️ Personalized Treatment Plans: Research shows that tailored treatment strategies yield better outcomes than one-size-fits-all approaches.
❌ Overgeneralizing Treatments: Not every treatment works for every patient; individual differences must be considered.
Table: Key Research Findings
| Research Focus | Finding | Impact on Treatment |
|---|---|---|
| Hormonal Imbalances | Correcting hormone levels can improve growth | Supports use of gonadotropins and hormonal supplements |
| Genetic Markers | Specific genes may be linked to abnormal growth | Can lead to more personalized treatments |
| Lifestyle Factors | Diet, exercise, and stress management matter | Encourages holistic and supportive care strategies |
Practical Advice for Patients
Lifestyle Changes That Can Help
Improving overall health can make a big difference in managing abnormal follicle development. Here are some practical tips:
-
Nutrition:
✔️ Eat plenty of fruits, vegetables, and whole grains.
✔️ Include sources of omega-3 fatty acids such as fish and walnuts.
❌ Avoid processed foods and excessive sugar, which can worsen inflammation. -
Exercise:
✔️ Engage in regular, moderate exercise like walking, swimming, or yoga.
✔️ Aim for at least 30 minutes a day to improve blood flow and reduce stress.
❌ Overexercising or high-intensity workouts that lead to exhaustion. -
Stress Reduction:
✔️ Practice relaxation techniques such as meditation, deep breathing, or mindfulness.
✔️ Consider activities like reading, listening to music, or spending time in nature.
❌ Letting stress build up without taking time to relax.
Dos and Don’ts: A Helpful Checklist
Checklist: Managing Abnormal Follicle Development
- Do:
- ✔️ Follow your doctor’s advice and treatment plan.
- ✔️ Keep a health diary to monitor changes.
- ✔️ Stay informed by reading reliable sources about fertility.
- ✔️ Practice stress management and self-care.
- Don’t:
- ❌ Ignore symptoms or skip follow-up appointments.
- ❌ Rely solely on the internet for advice—always consult a specialist.
- ❌ Overwhelm yourself with too many lifestyle changes at once.
Step-by-Step Guide to Managing Your Health
- Consult a Specialist:
- Begin with a thorough check-up and discussion about your symptoms.
- Undergo Diagnostic Tests:
- Get an ultrasound, hormone tests, and any other recommended evaluations.
- Develop a Personalized Plan:
- Work with your healthcare team to create a treatment plan tailored to you.
- Implement Lifestyle Changes:
- Adjust your diet, exercise routine, and stress management practices.
- Monitor Progress:
- Keep a diary and schedule regular follow-ups to assess improvements.
- Adjust as Needed:
- Make changes to your treatment plan based on feedback and test results.
Real Stories and Testimonials
Patient Success Stories
Real-life experiences can be incredibly reassuring. Here’s one example from a patient (name changed for privacy):
Case Study: Emily’s Journey
Emily had struggled with irregular cycles and painful symptoms for years. After a detailed evaluation, our team diagnosed her with abnormal follicle development. With a personalized treatment plan that combined medication, lifestyle changes, and regular monitoring, Emily began to see improvements. Her follicles started to develop more consistently, and her cycle regularity improved. Today, Emily is on a hopeful path toward achieving her dream of starting a family.
Checklist: What Helped Emily ✔️ Timely diagnosis and thorough testing
✔️ A tailored treatment plan addressing her specific needs
✔️ Regular follow-ups and adjustments to her care
❌ Rushing into one-size-fits-all treatments
Insights from Our Experts
Our team of doctors and fertility specialists shares their insights:
- Dr. Anderson: “Every patient is unique. Understanding the individual patterns of follicle development allows us to create a plan that really works. The key is personalized care.”
- Nurse Jessica: “We support our patients every step of the way. From explaining the tests to guiding them through lifestyle changes, our goal is to make the journey as smooth as possible.”
Core Explanation: The combination of personalized care and continuous support is critical to managing complex cases like abnormal follicle development.
Frequently Asked Questions (FAQ)
What is Abnormal Follicle Development?
Abnormal follicle development refers to a condition where the follicles in the ovaries do not grow or function as expected. This can lead to issues like irregular menstrual cycles, hormonal imbalances, and difficulty conceiving.
How Do You Know If You Have Abnormal Follicle Development?
Common signs include irregular cycles, lower quality eggs, or pain in the lower abdomen. A detailed ultrasound and hormone tests are essential for a proper diagnosis.
What Are the Treatment Options?
Treatment can include medication to balance hormones and stimulate follicle growth, lifestyle changes, and in some cases, surgical interventions. Each treatment is tailored to the patient’s specific situation.
How Long Does It Take to See Improvement?
The time frame can vary. With regular monitoring and personalized adjustments, some patients notice improvements within a few months, while others may require longer-term treatment.
Can Lifestyle Changes Really Make a Difference?
Yes, small adjustments in diet, exercise, and stress management can support overall ovarian health and help improve follicle development.
Is Abnormal Follicle Development Curable?
While the condition might not be “curable” in the traditional sense, many patients manage their symptoms effectively with the right treatment plan. This often leads to improved fertility and overall reproductive health.
Interactive Section: Share Your Story and Ask Questions
We want to hear from you! Your experiences and questions are important in building a supportive community. Here are some ways to join the conversation:
- Share Your Experience: Have you faced challenges with abnormal follicle development? Tell us your story in the comments section. Your insights could help someone else who is going through a similar journey.
- Ask a Question: Do you have questions about the diagnosis, treatment, or lifestyle changes? Leave your question below, and our team of experts will be happy to help.
- Participate in Our Poll: Would you like to see more detailed guides on specific treatments or lifestyle changes for abnormal follicle development? Vote in our poll and let us know your preferences.
Your feedback and interaction help us improve our content and create a more engaging, supportive space for everyone.
Conclusion and Final Thoughts
Abnormal follicle development is a complex issue that can impact your journey toward building a family. However, with the right diagnosis, personalized treatment, and ongoing support, it is possible to manage and improve this condition. Our story of helping Emily shows that a combination of careful testing, tailored treatments, and lifestyle changes can make a significant difference.
Key Takeaways:
- Understanding the Condition: Knowing what abnormal follicle development is and recognizing its symptoms is the first step.
- Personalized Diagnosis: A thorough, step-by-step diagnostic process helps identify the specific challenges.
- Tailored Treatment: Combining medication, lifestyle adjustments, and regular follow-up creates the best chance for improvement.
- Patient Support: Real-life success stories and expert insights remind us that you are not alone in this journey.
We hope this guide has given you a clear picture of what abnormal follicle development is and how a dedicated treatment plan can help. Your journey may be challenging, but with knowledge, support, and the right care, you can take control of your health and work toward a brighter future.
Interactive Challenge:
Write down one actionable tip from this article that you plan to implement in your life. Share your tip in the comments below and join our community discussion. Your feedback might inspire others to take the first step toward managing their own health challenges.
Thank you for reading our in-depth guide on a complex case of abnormal follicle development and how we helped. We invite you to subscribe to our newsletter for more updates, practical advice, and inspiring stories from others who have overcome similar obstacles. Together, we can build a supportive network and empower each other on the path to better health.
Remember, every small step counts. Whether you are starting your treatment or simply seeking more information, know that there is help available and many success stories to guide you along the way. Share this article with friends or family who might benefit, and let’s continue the conversation together.