The Case of Emily: Navigating Infertility Caused by Blocked Fallopian Tubes
Emily, a 33-year-old accountant, had been trying to conceive for two years when she walked into my clinic. She and her husband had tried everything—tracking ovulation, timing intercourse, even herbal remedies suggested by friends. Frustrated and emotionally drained, Emily finally decided to seek professional help.
Her case turned out to be a textbook example of how blocked fallopian tubes can silently disrupt fertility—and how modern medicine can help overcome this challenge.
Step 1: Understanding Blocked Fallopian Tubes
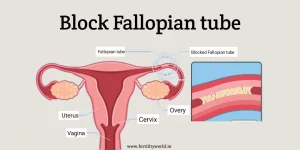
Blocked fallopian tubes are one of the leading causes of infertility in women. These tubes are critical for reproduction, serving as the passageway for eggs to travel from the ovaries to the uterus. When they are blocked, sperm can’t reach the egg, and fertilization cannot occur.
Emily had no obvious symptoms. She experienced regular periods and no pelvic pain. “How could my tubes be blocked if I feel normal?” she asked. I explained:
“Many women with blocked fallopian tubes have no symptoms until they try to conceive. That’s why it’s often called a ‘silent condition.’”
Step 2: Diagnosing the Problem
Emily’s fertility workup began with a standard evaluation. Initial blood tests showed normal hormone levels, and her ovulation was regular. Her husband’s semen analysis was also within normal limits.
To investigate further, I recommended a hysterosalpingography (HSG), an X-ray procedure that uses a contrast dye to check whether the fallopian tubes are open. The results were conclusive: both of Emily’s fallopian tubes were completely blocked near the uterine ends.
To confirm, we performed a laparoscopy—a minimally invasive surgery that allows us to visualize the tubes directly. During the procedure, we found evidence of pelvic scarring, likely caused by a mild, undiagnosed pelvic infection years earlier.
Step 3: Exploring Treatment Options
After her diagnosis, Emily wanted to know her options. I explained three potential paths:
1. Tubal Surgery
For some women, surgery to reopen the tubes can be effective. However, in Emily’s case, the blockages were severe, and the success rates for tubal surgery in such cases are relatively low. Additionally, the risk of ectopic pregnancy—where a fertilized egg implants in the tube instead of the uterus—would remain high.
2. In Vitro Fertilization (IVF)
IVF bypasses the fallopian tubes altogether, making it an ideal solution for women with bilateral tubal blockages. Eggs are retrieved directly from the ovaries, fertilized in a lab, and transferred into the uterus. This option offered Emily the best chance of success.
3. Watchful Waiting
For women with mild or partial blockages, lifestyle changes or anti-inflammatory treatments might improve fertility over time. However, Emily’s complete blockage made this approach unsuitable.
Emily chose IVF, and we began preparing her for the process.
Step 4: The IVF Process
IVF involves several steps, and Emily’s journey required precision and patience.
1. Ovarian Stimulation
Emily received daily hormone injections to stimulate her ovaries to produce multiple eggs. Frequent ultrasounds monitored her progress, ensuring her body responded appropriately to the medications.
2. Egg Retrieval
After two weeks, Emily’s eggs were mature and ready for retrieval. Using ultrasound guidance, we collected 12 eggs in a short outpatient procedure.
3. Fertilization and Embryo Development
Her husband’s sperm was used to fertilize the eggs in the lab. Of the 12 eggs, eight fertilized successfully, and five developed into high-quality embryos after five days of monitoring.
4. Embryo Transfer
One healthy embryo was transferred into Emily’s uterus. To improve implantation, Emily was prescribed progesterone supplements.
Step 5: Managing Emotional and Physical Challenges
Infertility treatments can be an emotional rollercoaster, and Emily’s journey was no exception. She often worried about the outcome, saying, “What if this doesn’t work?”
I reminded her:
“IVF is a process. Each step gets us closer to understanding your body and finding what works best.”
Emily also faced physical challenges, including mild ovarian hyperstimulation, a common side effect of IVF medications. With proper management, her symptoms subsided quickly.
Step 6: The Outcome
Two weeks after her embryo transfer, Emily took a pregnancy test—and it was positive. Her first ultrasound at six weeks confirmed a healthy pregnancy. Nine months later, Emily gave birth to a beautiful baby boy.
When she visited the clinic with her newborn, she said: “Thank you for helping me find hope when I thought there was none.”
Lessons from Emily’s Case
Emily’s story highlights critical insights about diagnosing and treating blocked fallopian tubes:
- Early Diagnosis Is Crucial:
Tests like HSG and laparoscopy can identify blockages and guide treatment decisions early. - Personalized Treatment Plans Matter:
Every woman’s case is unique. Surgery, IVF, or other approaches must be tailored to the individual. - Emotional Support Is Key:
Infertility is physically and emotionally challenging. Counseling and a supportive medical team can make a significant difference.
Expert Insights
Dr. Olivia Morgan, a reproductive specialist, explains:
“Blocked fallopian tubes are a significant cause of infertility, but they’re not the end of the road. Advances in fertility treatments like IVF have revolutionized how we address this issue, offering hope to many couples.”
Final Thoughts
If you’ve been diagnosed with blocked fallopian tubes, know that there are solutions. Whether it’s surgery, IVF, or another treatment, modern medicine offers a path forward. Emily’s journey shows that even the most challenging cases can end with the joy of parenthood.
Take the first step today—consult a specialist and explore your options. Your dream of a family is closer than you think.



