Male Infertility and Azoospermia: A Deep Dive into Causes, Solutions, and Hope
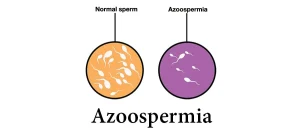
Male infertility can feel like a heavy burden, but understanding it is the first step toward finding solutions. One of the most challenging conditions tied to male infertility is azoospermia—a medical term that simply means no sperm is found in a man’s semen. If you or someone you love is facing this, you’re not alone. About 1% of all men and up to 15% of those struggling with infertility deal with azoospermia. Let’s break it down together—what it is, why it happens, and what you can do about it. This isn’t just another article; it’s a roadmap with fresh insights, practical advice, and the latest research to guide you.
What Is Azoospermia and Why Does It Matter?
Azoospermia sounds complicated, but it’s straightforward: it’s when a man’s semen has zero sperm. Normally, semen contains millions of tiny swimmers ready to fertilize an egg. With azoospermia, though, they’re missing in action. This condition is a big deal because it’s one of the top reasons men face infertility challenges. Without sperm, natural conception isn’t possible—but that doesn’t mean all hope is lost.
Two Main Types of Azoospermia
There are two kinds of azoospermia, and knowing which one you’re dealing with is key to figuring out the next steps:
- Obstructive Azoospermia (OA)
- What’s happening? The testicles are making sperm, but something’s blocking them from getting out—like a traffic jam in the reproductive system.
- How common is it? About 40% of azoospermia cases are obstructive.
- Causes: Past surgeries (like a vasectomy), infections, or birth defects like missing tubes (vas deferens).
- Non-Obstructive Azoospermia (NOA)
- What’s happening? The testicles aren’t producing sperm, or they’re making so little it doesn’t show up in the semen.
- How common is it? This covers about 60% of cases.
- Causes: Genetics, hormone issues, or damage from things like radiation or toxins.
Why It Matters to You
If you’re trying to start a family, azoospermia can feel like a roadblock. But here’s the good news: modern medicine has ways to tackle both types. Whether it’s clearing a blockage or finding a few hidden sperm, there’s hope. Let’s dig deeper into what might be causing this and how to spot it.
What Causes Azoospermia? Unpacking the Reasons
Azoospermia isn’t a one-size-fits-all problem. It’s more like a puzzle with different pieces—some you’re born with, others come from life experiences. Here’s a breakdown of the main culprits:
Obstructive Azoospermia Causes
- Blockages: Think of the tubes (like the vas deferens or epididymis) as highways for sperm. If they’re clogged or missing, sperm can’t travel. This might happen from:
- Infections like epididymitis.
- Injuries or surgeries (e.g., vasectomy or hernia repair gone wrong).
- Cystic fibrosis gene mutations—up to 80% of men with congenital bilateral absence of the vas deferens (CBAVD) have these.
- Low Semen Volume: If semen looks acidic (pH < 7.0) or has no fructose (a sugar sperm need), it could signal a blockage near the seminal vesicles.
Non-Obstructive Azoospermia Causes
- Genetic Issues: Your DNA can play a big role:
- Klinefelter Syndrome (47, XXY): An extra X chromosome messes with sperm production.
- Y Chromosome Microdeletions: Tiny missing pieces of the Y chromosome (AZF regions) can stop sperm from forming.
- New Gene Discoveries: Recent studies (2021) found mutations in the PNLDC1 gene linked to NOA, affecting how sperm develop.
- Hormone Problems: Sperm need a team of hormones—like testosterone and FSH (follicle-stimulating hormone)—to grow. If the pituitary gland or hypothalamus isn’t sending the right signals, production stalls.
- Lifestyle and Environment:
- Toxins (pesticides, heavy metals).
- Radiation or chemotherapy.
- Overheating the testicles (think hot tubs or tight clothing over years).
Underexplored Cause: Stress and Sperm Production
Here’s something not talked about enough: chronic stress. While most articles focus on physical causes, emerging research suggests stress hormones (like cortisol) might suppress sperm-making signals in the brain. A 2023 study hinted that men with high stress levels had lower sperm counts, though more research is needed to connect this directly to azoospermia.
How Do You Know If You Have Azoospermia? Signs and Diagnosis
Azoospermia doesn’t wave a red flag with obvious symptoms. Most guys only find out when they can’t conceive after a year of trying. But there are clues and tests to get answers.
Signs to Watch For
- Infertility: The big one—trying for a baby with no luck.
- Low Semen Volume: Less than 1.5 mL could hint at a blockage.
- Other Hints: Smaller testicles, less body hair, or even breast tissue growth (gynecomastia) might point to hormone issues.
How Doctors Diagnose It
Doctors use a step-by-step approach to confirm azoospermia and figure out why:
- Semen Analysis (Step 1):
- You provide a sample (yep, in a cup). They spin it in a centrifuge to check for any sperm. If none show up twice, it’s azoospermia.
- Tip: Avoid ejaculation for 2-5 days before the test for accurate results.
- Physical Exam (Step 2):
- The doctor checks your testicles, vas deferens, and looks for varicoceles (swollen veins).
- Hormone Tests (Step 3):
- Blood tests measure FSH, testosterone, and more. High FSH might mean the testicles aren’t working; low levels could point to a brain signal issue.
- Genetic Testing (Step 4):
- Karyotyping checks chromosomes; Y-chromosome testing looks for microdeletions.
- Imaging (Step 5):
- A scrotal ultrasound or MRI can spot blockages or structural problems.
Interactive Quiz: Could It Be Azoospermia?
Take a quick self-check (not a diagnosis—just a guide!):
- ✔️ Have you been trying to conceive for over a year with no success?
- ✔️ Is your semen volume noticeably low?
- ✔️ Do you have a history of infections, surgeries, or genetic conditions in the family? If you checked two or more, talk to a doctor about testing!
Treatments for Azoospermia: What Are Your Options?
Here’s where hope shines through. Azoospermia isn’t a dead end—treatments depend on the type and cause. Let’s explore your options.
Fixing Obstructive Azoospermia
- Surgery:
- What: Reconnect blocked tubes or remove obstructions.
- Success Rate: Up to 90% of men restore sperm flow after vasectomy reversal.
- Example: Microsurgery fixes epididymal blockages.
- Sperm Retrieval:
- What: Doctors extract sperm directly from the testicles or epididymis using techniques like TESE (Testicular Sperm Extraction) or MESA (Microsurgical Epididymal Sperm Aspiration).
- Next Step: Use the sperm with IVF/ICSI (more on that below).
Tackling Non-Obstructive Azoospermia
- Hormone Therapy:
- What: Boost hormones with drugs like hCG or clomiphene if levels are off.
- Who It Helps: Men with hypogonadotropic hypogonadism (low brain signals).
- Results: A 2024 study showed 68% of men with this condition saw sperm return after hCG therapy.
- Sperm Retrieval for IVF:
- What: Even with NOA, tiny amounts of sperm might hide in the testicles. TESE can find them in up to 50% of cases.
- Catch: Genetic issues like AZFa deletions make retrieval unlikely.
- Donor Sperm or Adoption: If no sperm are found, these are valid paths to parenthood.
IVF and ICSI: The Game-Changers
- How It Works:
- IVF (In Vitro Fertilization) mixes sperm and egg in a lab. ICSI (Intracytoplasmic Sperm Injection) takes it further by injecting one sperm directly into an egg.
- Success: With retrieved sperm, ICSI boasts pregnancy rates of 30-40% per cycle.
- Real Story: John, 35, had OA from a childhood infection. Doctors retrieved sperm via TESE, used ICSI, and he’s now a dad to twins!
New Frontiers: Cutting-Edge Research and Treatments
Most articles stop at standard treatments, but let’s push further. Here are three areas not fully covered elsewhere:
1. Platelet-Rich Plasma (PRP) Therapy
- What Is It? PRP uses your blood’s growth factors to stimulate tissue repair. Early studies (2024) suggest injecting it into testicles might boost sperm production in NOA.
- Evidence: Small trials show improved sperm retrieval rates, but it’s experimental.
- Action Step: Ask your doctor about PRP clinical trials near you.
2. Stem Cell Therapy
- What’s Happening? Scientists are turning stem cells into sperm precursors in labs. A 2023 mouse study succeeded in creating functional sperm this way.
- Future Hope: Human trials are years off, but this could revolutionize NOA treatment.
- Stay Tuned: Follow research updates from groups like the NIH.
3. Full-Field Optical Coherence Tomography (FFOCT)
- What Is It? A new imaging tool that spots live sperm in testicular tissue during surgery—better than traditional biopsies.
- Why It’s Cool: It could make TESE more precise, upping success rates.
- Where It’s At: Still in testing, but watch for it in advanced fertility clinics.
Practical Tips: What You Can Do Right Now
You don’t have to wait for a doctor’s appointment to take action. Here’s how to support your fertility today:
Lifestyle Changes
- ✔️ Cool It Down: Skip hot tubs and tight pants—keep testicles at 94-96°F.
- ✔️ Eat Smart: Load up on antioxidants (berries, nuts, spinach) to fight oxidative stress.
- ❌ Cut Toxins: Quit smoking, limit alcohol, and avoid pesticides.
- ✔️ Move More: Exercise 3-4 times a week boosts testosterone.
Stress Management (The Overlooked Factor)
- ✔️ Try Mindfulness: A 10-minute daily meditation can lower cortisol.
- ❌ Don’t Bottle It Up: Talk to a friend or therapist about infertility stress.
Step-by-Step Plan to Get Started
- Track Symptoms: Note semen volume, energy levels, or libido changes.
- See a Urologist: Ask for a semen analysis and hormone tests.
- Genetic Check: If azoospermia is confirmed, push for karyotyping or CFTR testing.
- Explore Options: Discuss surgery, retrieval, or IVF with a fertility specialist.
Emotional Side of Azoospermia: Coping and Connecting
Infertility isn’t just physical—it’s emotional. Men often feel shame or failure, but you’re not alone, and it’s not your fault.
Real Talk: How It Feels
- Mike, 32: “I felt like less of a man when I got the diagnosis. Talking to my wife helped me see it’s a team effort.”
- Stats: Studies show 20-30% of infertile men experience anxiety or depression.
Coping Strategies
- ✔️ Join a Group: Online forums (like Reddit’s r/infertility) offer support.
- ✔️ Educate Yourself: Knowledge (like this article!) reduces fear.
- ❌ Avoid Blame: It’s a medical issue, not a personal flaw.
Poll: How Do You Handle It?
What helps you cope with infertility stress?
- A) Talking to loved ones
- B) Exercise or hobbies
- C) Professional support
Share in the comments—I’ll tally the votes!
Busting Myths: What Azoospermia Isn’t
Misinformation spreads fast. Let’s clear up some common myths:
- ❌ Myth: “Azoospermia means you’re sterile forever.”
Truth: Many men conceive with treatment. - ❌ Myth: “It’s always genetic.”
Truth: Lifestyle and blockages play roles too. - ❌ Myth: “Low testosterone causes it.”
Truth: Testosterone helps, but it’s not the whole story.
Your Next Steps: A Roadmap to Parenthood
Azoospermia might feel overwhelming, but you’ve got options and a path forward. Here’s a quick guide:
If You Suspect Azoospermia
- Get tested ASAP—don’t wait.
- Gather your medical history (surgeries, infections, family issues).
If You’re Diagnosed
- OA: Explore surgery or retrieval + IVF.
- NOA: Try hormone therapy or TESE; consider donor sperm if needed.
- Talk costs—IVF can run $10,000-$15,000 per cycle, but insurance might help.
Unique Insight: Mini Fertility Audit
Try this at home:
- ✔️ Check your semen volume with a measuring spoon (normal is 1.5-6 mL).
- ✔️ Feel your testicles—are they smaller than a walnut?
- ✔️ Rate your stress (1-10). High scores? Time to act.
Share your results with your doctor for a head start!
Final Thoughts: You’ve Got This
Azoospermia is a tough diagnosis, but it’s not the end of your story. With today’s science—surgery, IVF, and even experimental treatments like PRP—plus small lifestyle tweaks, you’re closer to your goals than you think. This isn’t just about facts; it’s about hope, action, and knowing you’re not alone. What’s your next step? Drop a comment—I’m here to cheer you on!



