Endometriosis: A Deep Dive into a Hidden Condition
Endometriosis affects millions of women, yet many don’t even know they have it. It’s a condition that can cause pain, disrupt daily life, and make it hard to get pregnant. Let’s explore what endometriosis is, how it affects the body, and what can be done about it.
What Exactly Is Endometriosis?
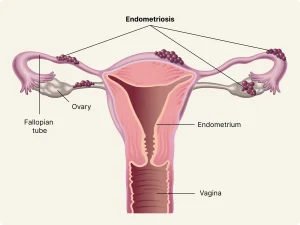
Endometriosis happens when tissue similar to the lining of the uterus starts growing outside of it. This rogue tissue can show up on the ovaries, fallopian tubes, and other areas in the pelvis. Dr. Lisa Thompson, a leading gynecologist, explains, “Imagine bits of the uterine lining spreading where they shouldn’t, causing irritation and pain.”
Common Symptoms to Watch For
Endometriosis can be tricky because symptoms vary. Some women have severe pain, while others feel nothing at all. Here are common signs:
- Painful Periods: Cramps that are worse than usual.
- Chronic Pelvic Pain: Ongoing discomfort in the lower abdomen or back.
- Pain During or After Sex: Discomfort that isn’t normal.
- Heavy Bleeding: Periods that are heavier or last longer than usual.
- Digestive Issues: Bloating, constipation, or nausea, especially during periods.
- Trouble Getting Pregnant: Difficulty conceiving might be a sign.
Dr. Maria Gonzalez points out, “Many women think painful periods are normal, but extreme pain isn’t something you should ignore.”
What Causes Endometriosis?
The exact cause isn’t known, but there are several theories:
- Retrograde Menstruation: Menstrual blood flows back through the fallopian tubes into the pelvic cavity.
- Hormonal Factors: Estrogen might promote the growth of endometrial tissue.
- Immune System Disorders: The body might not detect and destroy endometrial-like tissue outside the uterus.
- Genetics: It can run in families.
How Does Endometriosis Affect Fertility?
Endometriosis can make it harder to get pregnant. The misplaced tissue can cause:
- Scar Tissue and Adhesions: These can block the fallopian tubes.
- Inflammation: Creates a hostile environment for eggs and sperm.
- Altered Egg Quality: Ovarian endometriomas (cysts) can affect the health of eggs.
Dr. Karen Lee, a fertility specialist, says, “Endometriosis is one of the leading causes of infertility, but treatments are available that offer hope.”
Diagnosing Endometriosis
Finding out if you have endometriosis can be a journey. Here’s how doctors figure it out:
- Symptom Review: Discussing pain levels and menstrual cycles.
- Pelvic Exam: Feeling for cysts or scars.
- Ultrasound: Using sound waves to create images of the reproductive organs.
- MRI Scans: Detailed images to spot endometrial tissue.
- Laparoscopy: A minor surgery where a tiny camera looks inside the pelvis. This is the only way to confirm endometriosis for sure.
Treatment Options
While there’s no cure, treatments can manage symptoms and improve fertility.
- Pain Relief
- Over-the-Counter Medications: Like ibuprofen.
- Prescription Painkillers: For more severe pain.
- Hormone Therapy
- Birth Control Pills: Regulate hormones and reduce or eliminate periods.
- GnRH Agonists: Medications that lower estrogen levels.
- Progestin Therapy: Helps stop menstrual periods and growth of endometrial tissue.
- Surgical Options
- Laparoscopic Surgery: Removes as much endometrial tissue as possible.
- Hysterectomy: Removal of the uterus and possibly ovaries, considered a last resort.
- Assisted Reproductive Technologies
- In Vitro Fertilization (IVF): Bypasses many of the problems caused by endometriosis.
- Egg Freezing: Preserves fertility for future use.
Dr. Thompson emphasizes, “Treatment should be tailored to each woman, depending on her symptoms and desire to have children.”
Lifestyle Changes to Manage Symptoms
Small changes can make a big difference.
- Diet Adjustments
- Anti-Inflammatory Foods: Eat more fruits, vegetables, and whole grains.
- Limit Caffeine and Alcohol: They might worsen symptoms.
- Regular Exercise
- Stay Active: Helps reduce estrogen levels and ease pain.
- Stress Reduction
- Mindfulness and Relaxation Techniques: Yoga or meditation can help.
Dr. Gonzalez advises, “Listening to your body and making healthy choices can complement medical treatments.”
Emotional Well-being and Support
Endometriosis isn’t just physical; it can take an emotional toll.
- Seek Support Groups: Connecting with others can provide comfort.
- Counseling: Talking to a professional about feelings of frustration or anxiety.
- Open Communication: Sharing your experience with friends and family.
Dr. Lee reminds us, “You’re not alone, and it’s okay to ask for help.”
Looking Ahead: Hope for the Future
Research is ongoing to find better treatments and eventually a cure.
- New Medications: Studies are testing drugs that target endometrial tissue more effectively.
- Improved Surgical Techniques: Less invasive methods with quicker recovery times.
- Greater Awareness: Education helps women get diagnosed earlier.
Conclusion
Endometriosis is a complex condition, but understanding it empowers you to take action. Whether it’s managing pain, exploring fertility options, or making lifestyle changes, there are steps you can take. As Dr. Thompson says, “Knowledge is the first step toward taking control of your health.”
If you think you might have endometriosis, don’t hesitate to talk to a healthcare professional. Early diagnosis and treatment can improve your quality of life and open doors to starting a family.
FAQ:
- What are the different stages of endometriosis?
Endometriosis is classified into four stages (minimal, mild, moderate, and severe) based on the location, amount, depth, and size of endometrial implants. - Is endometriosis the same as fibroids?
No, endometriosis involves endometrial-like tissue growing outside the uterus, while fibroids are noncancerous growths within the uterus itself. - Can endometriosis cause gastrointestinal issues?
Yes, endometrial tissue near the intestines can cause symptoms like bloating, constipation, and nausea, especially during menstruation. - Is there a link between endometriosis and autoimmune diseases?
Some studies suggest a potential link, as both involve the immune system, but more research is needed to confirm this connection. - Can birth control pills help manage endometriosis?
Yes, hormonal birth control can help manage symptoms by regulating hormones and reducing menstrual flow. - How long does it typically take to diagnose endometriosis?
Diagnosis can be delayed by several years, as symptoms are often mistaken for other conditions, leading to an average delay of 7-10 years. - Are there specific exercises that help with endometriosis pain?
Gentle exercises like yoga, stretching, and low-impact cardio can help relieve pain and reduce inflammation. - Does endometriosis get worse over time?
In some cases, endometriosis can progress, but the rate of progression varies among individuals. - Can endometriosis affect menstruation cycles?
Yes, it often leads to heavy, irregular, or prolonged periods, depending on the severity and location of tissue growth. - Is hormone replacement therapy safe for women with endometriosis?
Hormone therapy post-menopause can sometimes reactivate endometriosis, so it’s best managed under a doctor’s care. - Are natural remedies effective in treating endometriosis?
While natural approaches like herbal supplements and acupuncture may provide symptom relief, they should be used alongside medical treatments. - Can endometriosis recur after surgery?
Yes, endometrial tissue can regrow, and symptoms may return after surgery, though this varies by individual. - Does endometriosis increase the risk of miscarriage?
Some studies suggest a higher risk of miscarriage for women with endometriosis, although the exact reasons aren’t fully understood. - Is endometriosis associated with chronic fatigue?
Many women with endometriosis report fatigue, which may be due to chronic pain, inflammation, and hormonal changes. - Does stress worsen endometriosis symptoms?
While stress doesn’t cause endometriosis, it can exacerbate pain and make symptoms feel more intense. - Can pregnancy help alleviate endometriosis symptoms?
Pregnancy often reduces symptoms due to the hormonal changes that suppress menstruation, but this relief may be temporary. - How does endometriosis affect sex life?
Pain during intercourse is a common symptom, which can impact intimacy and emotional health. - Are there specific tests that predict the likelihood of developing endometriosis?
Currently, no tests can predict endometriosis risk, but a family history can be a strong indicator. - Can lifestyle changes help manage endometriosis long-term?
Yes, diet, exercise, and stress management can all play a role in managing symptoms and improving quality of life.



